Clin Endosc.
2016 May;49(3):289-293. 10.5946/ce.2015.092.
Gastrointestinal Endoscopy-Assisted Minimally Invasive Surgery for Superficial Cancer of the Uvula
- Affiliations
-
- 1Department of Gastroenterology, Saiseikai Kawaguchi General Hospital, Saitama, Japan. hodagiri-gi@umin.ac.jp
- 2Department of Clinical Epidemiology and Health Economics, The University of Tokyo School of Public Health, Tokyo, Japan.
- 3Department of Gastroenterology, Toranomon Hospital, Tokyo, Japan.
- 4Department of Otolaryngology, Toranomon Hospital, Tokyo, Japan.
- 5Department of Pathology, Graduate School of Medicine, Yokohama City University, Yokohama, Japan.
- KMID: 2165024
- DOI: http://doi.org/10.5946/ce.2015.092
Abstract
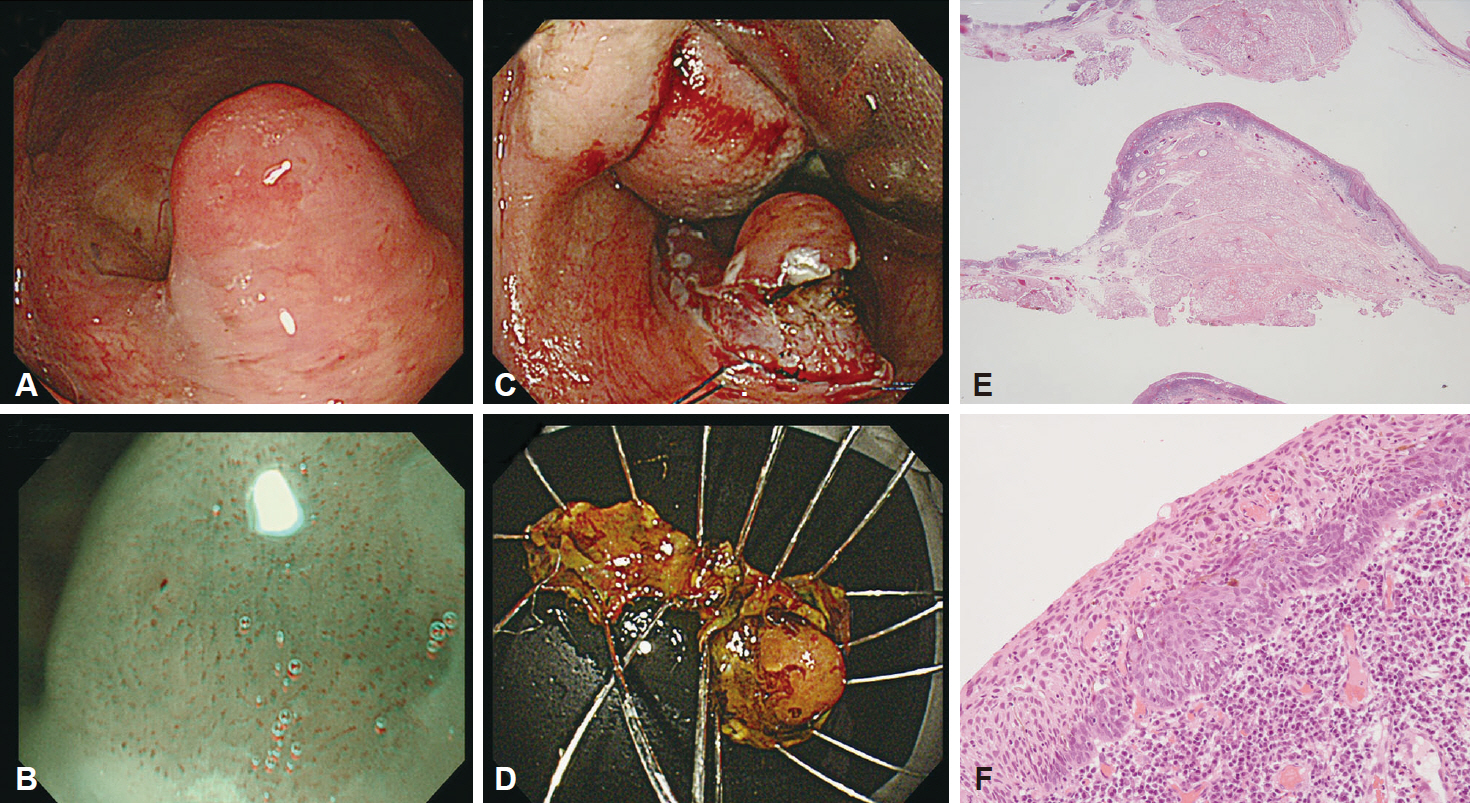
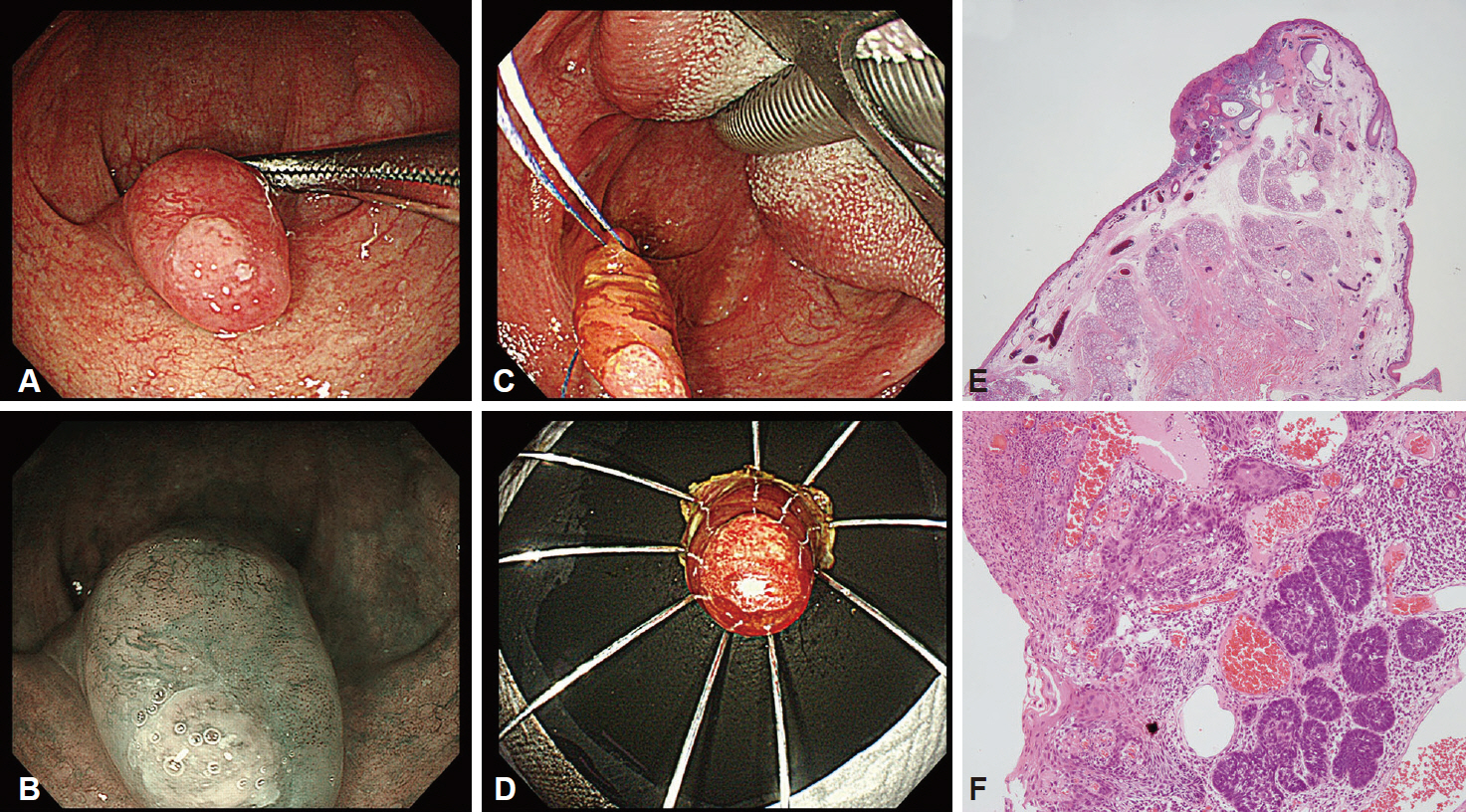
- Previous studies reported that endoscopic resection is effective for the treatment of superficial pharyngeal cancers, as for digestive tract cancers. However, the optimal treatment for superficial cancer of the uvula has not been established because of the rarity of this condition. We present two male patients in their 70s with superficial cancer of the uvula, detected with upper gastrointestinal endoscopy. Both patients underwent surgical resection of the uvula under general anesthesia. The extent of the lesions was determined by means of gastrointestinal endoscopy by using magnifying observation with narrow-band imaging, enabling the performance of minimally invasive surgery. Endoscopic submucosal dissection was performed to achieve en bloc resection of the intramucosal carcinoma that had infiltrated the area adjacent to the uvula. Gastrointestinal endoscopists should carefully examine the laryngopharynx to avoid missing superficial cancers. Our minimally invasive treatment for superficial cancer of the uvula had favorable postoperative outcomes, and prevented postoperative loss of breathing, swallowing, and articulation functions.
Keyword
MeSH Terms
Figure
Reference
-
1. Okada K, Tsuchida T, Ishiyama A, et al. Endoscopic mucosal resection and endoscopic submucosal dissection for en bloc resection of superficial pharyngeal carcinomas. Endoscopy. 2012; 44:556–564.
Article2. Wahlberg PC, Andersson KE, Biörklund AT, Möller TR. Carcinoma of the hypopharynx: analysis of incidence and survival in Sweden over a 30-year period. Head Neck. 1998; 20:714–719.
Article3. Johansen LV, Grau C, Overgaard J. Hypopharyngeal squamous cell carcinoma: treatment results in 138 consecutively admitted patients. Acta Oncol. 2000; 39:529–536.4. Eckel HE, Staar S, Volling P, Sittel C, Damm M, Jungehuelsing M. Surgical treatment for hypopharynx carcinoma: feasibility, mortality, and results. Otolaryngol Head Neck Surg. 2001; 124:561–569.
Article5. Muto M, Nakane M, Katada C, et al. Squamous cell carcinoma in situ at oropharyngeal and hypopharyngeal mucosal sites. Cancer. 2004; 101:1375–1381.
Article6. Muto M, Minashi K, Yano T, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010; 28:1566–1572.
Article7. Shimizu Y, Yamamoto J, Kato M, et al. Endoscopic submucosal dissection for treatment of early stage hypopharyngeal carcinoma. Gastrointest Endosc. 2006; 64:255–259.
Article8. Iizuka T, Kikuchi D, Hoteya S, Yahagi N, Takeda H. Endoscopic submucosal dissection for treatment of mesopharyngeal and hypopharyngeal carcinomas. Endoscopy. 2009; 41:113–117.
Article9. Hanaoka N, Ishihara R, Takeuchi Y, et al. Clinical outcomes of endoscopic mucosal resection and endoscopic submucosal dissection as a transoral treatment for superficial pharyngeal cancer. Head Neck. 2013; 35:1248–1254.
Article10. Kuwabara T, Hiyama T, Oka S, et al. Clinical features of pharyngeal intraepithelial neoplasias and outcomes of treatment by endoscopic submucosal dissection. Gastrointest Endosc. 2012; 76:1095–1103.
Article11. Japan Society for Head and Neck Cancer. Classification of Head and Neck Carcinoma. 5th ed. Tokyo: Kanehara-Syuppan;2012.12. Kraus DH, Zelefsky MJ, Brock HA, Huo J, Harrison LB, Shah JP. Combined surgery and radiation therapy for squamous cell carcinoma of the hypopharynx. Otolaryngol Head Neck Surg. 1997; 116(6 Pt 1):637–641.
Article13. Shimizu Y, Tsukagoshi H, Fujita M, et al. Head and neck cancer arising after endoscopic mucosal resection for squamous cell carcinoma of the esophagus. Endoscopy. 2003; 35:322–326.
Article14. Muto M, Satake H, Yano T, et al. Long-term outcome of transoral organ-preserving pharyngeal endoscopic resection for superficial pharyngeal cancer. Gastrointest Endosc. 2011; 74:477–484.
Article15. Hemminki K, Boffetta P. Multiple primary cancers as clues to environmental and heritable causes of cancer and mechanisms of carcinogenesis. IARC Sci Publ. 2004; 157:289–297.16. Inoue H, Honda T, Nagai K, et al. Ultra-high magnification endoscopic observation of carcinoma in situ of the esophagus. Dig Endosc. 1997; 9:16–18.
Article17. Kumagai Y, Inoue H, Nagai K, Kawano T, Iwai T. Magnifying endoscopy, stereoscopic microscopy, and the microvascular architecture of superficial esophageal carcinoma. Endoscopy. 2002; 34:369–375.
Article18. Espinosa Restrepo F, Martínez Capoccioni G, Martín Martín C. T1-T2 squamous cell carcinoma of the uvula: a little big enemy. Otolaryngol Head Neck Surg. 2012; 146:81–87.19. Calais G, Goga D, Chauvet B, Carand G, Beutter P, Le Floch O. Carcinoma of the soft palate and uvula. An analysis of the results and the reasons for failures: a study of 76 cases. Rev Stomatol Chir Maxillofac. 1988; 89:306–310.20. Imai K, Tanaka M, Hasuike N, et al. Feasibility of a “resect and watch” strategy with endoscopic resection for superficial pharyngeal cancer. Gastrointest Endosc. 2013; 78:22–29.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Establishment of Minimally Invasive Thoracic Surgery Program
- Comments on “Impact of nasogastric tube exclusion after minimally invasive esophagectomy for esophageal cancer: a single-center retrospective study in India”
- Natural Orifice Transluminal Endoscopic Surgery in Korea
- A New Beginning for the Journal of Minimally Invasive Surgery for the International Recognition and Contribution of Scientific Development of Minimally Invasive Surgery
- Minimally Invasive Thoracic Surgery in Lung Cancer Operation