Yonsei Med J.
2015 Sep;56(5):1428-1436. 10.3349/ymj.2015.56.5.1428.
The Long-Term Effect of an Independent Capacity Protocol on Emergency Department Length of Stay: A before and after Study
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Medical Center, Seoul, Korea.
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. shinsangdo@medimail.co.kr
- 3Department of Emergency Medicine, Gachon University Gil Hospital, Seoul, Korea.
- 4Department of Emergency Medicine, Stony Brook University, NY, USA.
- KMID: 2163640
- DOI: http://doi.org/10.3349/ymj.2015.56.5.1428
Abstract
- PURPOSE
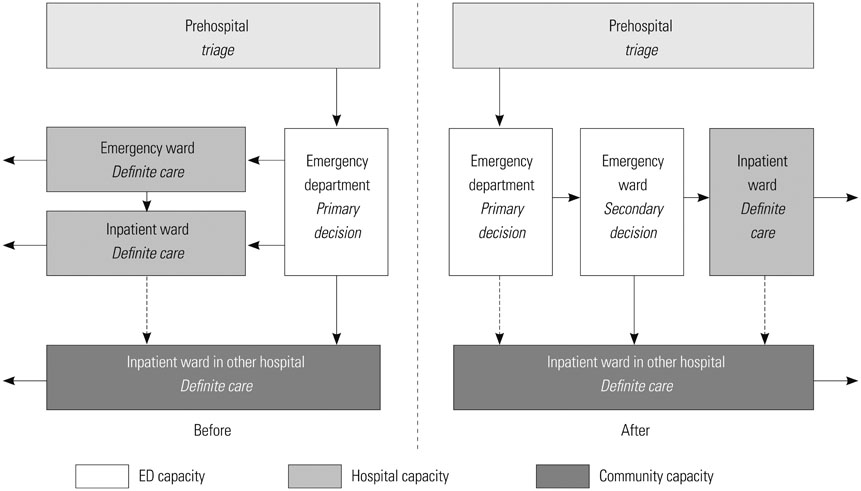
In this study, we determined the long-term effects of the Independent Capacity Protocol (ICP), in which the emergency department (ED) is temporarily used to stabilize patients, followed by transfer of patients to other facilities when necessary, on crowding metrics.
MATERIALS AND METHODS
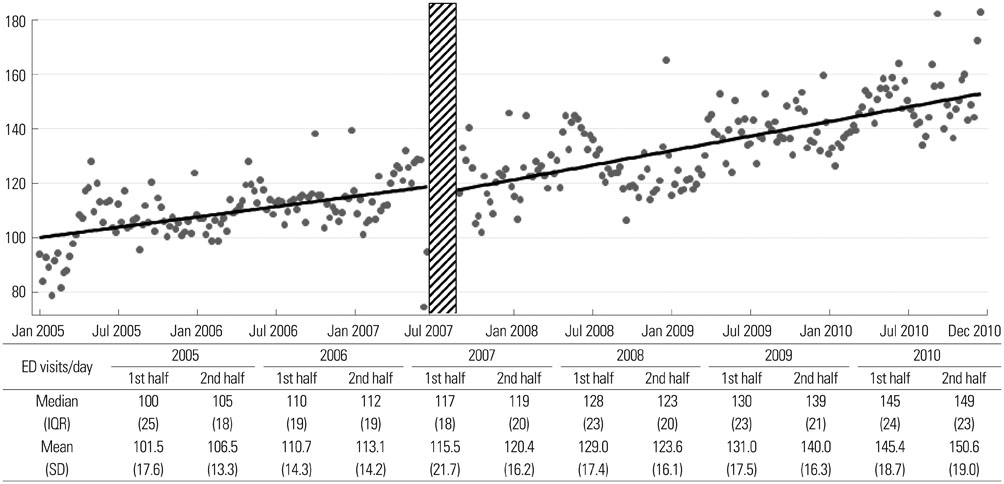
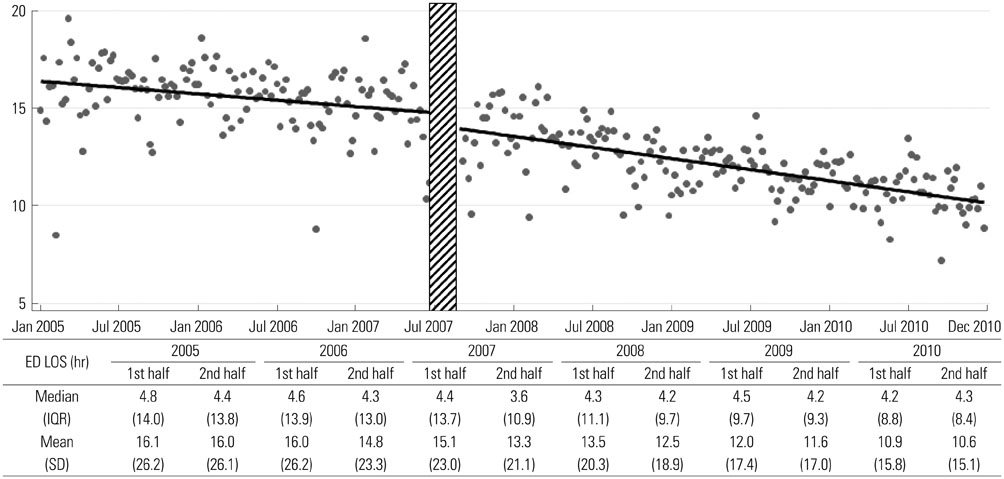
A before and after study design was used to determine the effects of the ICP on patient outcomes in an academic, urban, tertiary care hospital. The ICP was introduced on July 1, 2007 and the before period included patients presenting to the ED from January 1, 2005 to June 31, 2007. The after period began three months after implementing the ICP from October 1, 2007 to December 31, 2010. The main outcomes were the ED length of stay (LOS) and the total hospital LOS of admitted patients. The mean number of monthly ED visits and the rate of inter-facility transfers between emergency departments were also determined. A piecewise regression analysis, according to observation time intervals, was used to determine the effect of the ICP on the outcomes.
RESULTS
During the study period the number of ED visits significantly increased. The intercept for overall ED LOS after intervention from the before-period decreased from 8.51 to 7.98 hours [difference 0.52, 95% confidence interval (CI): 0.04 to 1.01] (p=0.03), and the slope decreased from -0.0110 to -0.0179 hour/week (difference 0.0069, 95% CI: 0.0012 to 0.0125) (p=0.02).
CONCLUSION
Implementation of the ICP was associated with a sustainable reduction in ED LOS and time to admission over a six-year period.
Keyword
MeSH Terms
-
Aged
*Clinical Protocols
*Crowding
Efficiency, Organizational
Emergency Service, Hospital/*organization & administration/utilization
Female
Hospital Planning/*methods
Hospitals, Urban/*organization & administration/utilization
Humans
Length of Stay/*statistics & numerical data
Male
Outcome and Process Assessment (Health Care)
Patient Admission/statistics & numerical data
Patient Transfer/statistics & numerical data
Regression Analysis
Time
Time Factors
Triage
Figure
Reference
-
1. Shih FY, Ma MH, Chen SC, Wang HP, Fang CC, Shyu RS, et al. ED overcrowding in Taiwan: facts and strategies. Am J Emerg Med. 1999; 17:198–202.
Article2. Li G, Lau JT, McCarthy ML, Schull MJ, Vermeulen M, Kelen GD. Emergency department utilization in the United States and Ontario, Canada. Acad Emerg Med. 2007; 14:582–584.
Article3. Anantharaman V. Impact of health care system interventions on emergency department utilization and overcrowding in Singapore. Int J Emerg Med. 2008; 1:11–20.
Article4. Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011; 18:1358–1370.
Article5. Canadian Association of Emergency Physicians. National Emergency Nurses Affiliation. Joint Position Statement on emergency department overcrowding. CJEM. 2001; 3:82–88.6. Walsh P, Cortez V, Bhakta H. Patients would prefer ward to emergency department boarding while awaiting an inpatient bed. J Emerg Med. 2008; 34:221–226.
Article7. Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001; 8:151–155.
Article8. Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009; 16:1–10.
Article9. Singer AJ, Thode HC Jr, Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011; 18:1324–1329.
Article10. Liu SW, Chang Y, Weissman JS, Griffey RT, Thomas J, Nergui S, et al. An empirical assessment of boarding and quality of care: delays in care among chest pain, pneumonia, and cellulitis patients. Acad Emerg Med. 2011; 18:1339–1348.
Article11. Cha WC, Shin SD, Cho JS, Song KJ, Singer AJ, Kwak YH. The association between crowding and mortality in admitted pediatric patients from mixed adult-pediatric emergency departments in Korea. Pediatr Emerg Care. 2011; 27:1136–1141.
Article12. Pham JC, Patel R, Millin MG, Kirsch TD, Chanmugam A. The effects of ambulance diversion: a comprehensive review. Acad Emerg Med. 2006; 13:1220–1227.13. Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006; 1–23.14. Hsia RY, Asch SM, Weiss RE, Zingmond D, Liang LJ, Han W, et al. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med. 2011; 58:24–32.
Article15. Cha WC, Shin SD, Song KJ, Jung SK, Suh GJ. Effect of an independent-capacity protocol on overcrowding in an urban emergency department. Acad Emerg Med. 2009; 16:1277–1283.16. Richards JR, Ozery G, Notash M, Sokolove PE, Derlet RW, Panacek EA. Patients prefer boarding in inpatient hallways: correlation with the national emergency department overcrowding score. Emerg Med Int. 2011; 2011:840459.
Article17. Viccellio A, Santora C, Singer AJ, Thode HC Jr, Henry MC. The association between transfer of emergency department boarders to inpatient hallways and mortality: a 4-year experience. Ann Emerg Med. 2009; 54:487–491.18. Schneider SM, Asplin BR. Global crowding: opportunities for regionalization in emergency care. Acad Emerg Med. 2009; 16:1333–1334.
Article19. McConnell KJ, Richards CF, Daya M, Bernell SL, Weathers CC, Lowe RA. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005; 45:471–478.
Article20. Howell E, Bessman E, Kravet S, Kolodner K, Marshall R, Wright S. Active bed management by hospitalists and emergency department throughput. Ann Intern Med. 2008; 149:804–811.
Article21. Ahn KO, Shin SD, Cha WC, Jun C, Lee TS, Pirrallo RG. A model for the association of the call volume and the unavailable-for-response interval on the delayed ambulance response for out-of-hospital cardiac arrest using a geographic information system. Prehosp Emerg Care. 2010; 14:469–476.
Article22. Hwang SO, Lee CC, Singer AJ, Kim TM. The current status of the emergency medical system in Korea. Am J Emerg Med. 2007; 25:846–848.
Article23. Weiss SJ, Ernst AA, Nick TG. Comparison of the National Emergency Department Overcrowding Scale and the Emergency Department Work Index for quantifying emergency department crowding. Acad Emerg Med. 2006; 13:513–518.24. Bernstein SL, Verghese V, Leung W, Lunney AT, Perez I. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med. 2003; 10:938–942.
Article25. McCarthy ML, Aronsky D, Jones ID, Miner JR, Band RA, Baren JM, et al. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008; 51:15–24.26. Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000; 320:1197–1200.
Article27. Katz MH. Evaluating clinical and public health interventions. A practical guide to study design and statistcis. Cambridge: Cambridge University Press;2010. p. 128–132.28. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA Jr. A conceptual model of emergency department crowding. Ann Emerg Med. 2003; 42:173–180.
Article29. Han JH, Zhou C, France DJ, Zhong S, Jones I, Storrow AB, et al. The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med. 2007; 14:338–343.
Article30. Carr BG, Asplin BR. 2010 Academic Emergency Medicine consensus conference, Beyond Regionalization: Integrated Networks of Care. Regionalization and emergency care: the institute of medicine reports and a federal government update. Acad Emerg Med. 2010; 17:1351–1353.31. National Emergency Medical Center. National Emergency Department Information System. accessed on 2015 July 1. Available at: http://www.nemc.or.kr/egen/inf.emsin13.do.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Issuing of Hospitalization Sheets by Emergency Department on Shortening Length of Stay
- An Experience of Operating the Pediatric Emergency Room
- Stool White-cell Count as a Predictor of Long-term Admission in Healthy Patients with Acute Diarrhea
- Analysis of Factors Affecting Length of Hospital Stay in Geriatric Patients Transferred from Long-term Care Hospitals
- Factors Affecting the Length of Stay of Long-Stay Medical Aid Inpatients in Korea: Focused on Hospitalization Types in Long-Term Care Hospitals