Focal Lymphocytic Thyroiditis Nodules Share the Features of Papillary Thyroid Cancer on Ultrasound
- Affiliations
-
- 1Division of Endocrinology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. ejlee423@yuhs.ac
- 2Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 4Brain Korea 21 PLUS Project for Medical Science, Yonsei University, Seoul, Korea.
- KMID: 2163626
- DOI: http://doi.org/10.3349/ymj.2015.56.5.1338
Abstract
- PURPOSE
It is often difficult to discriminate focal lymphocytic thyroiditis (FLT) or adenomatous hyperplasia (AH) from thyroid cancer if they both have suspicious ultrasound (US) findings. We aimed to make a predictive model of FLT from papillary thyroid cancer (PTC) in suspicious nodules with benign cytologic results.
MATERIALS AND METHODS
We evaluated 214 patients who had undergone fine-needle aspiration biopsy (FNAB) and had shown thyroid nodules with suspicious US features. PTC was confirmed by surgical pathology. FLT and AH were confirmed through more than two separate FNABs. Clinical and biochemical findings, as well as US features, were evaluated.
RESULTS
Of 214 patients, 100 patients were diagnosed with PTC, 55 patients with FLT, and 59 patients with AH. The proportion of elevated thyrotropin (TSH) levels (p=0.014) and thyroglobulin antibody (Tg-Ab) or thyroid peroxidase antibody (TPO-Ab) positivity (p<0.001) in the FLT group was significantly higher than that in the PTC group. Regarding US features, absence of calcification (p=0.006) and "diffuse thyroid disease" (DTD) pattern on US (p<0.001) were frequently seen in the FLT group. On multivariate analysis, Tg-Ab positivity, presence of a DTD pattern on US, and absence of calcification in nodules were associated with FLT with the best specificity of 99% and positive predictive value of 96%. In contrast, a taller than wide shape of nodules was the only variable significant for differentiating AH from PTC.
CONCLUSION
Suspicious thyroid nodules with cytologic benign results could be followed up with US rather than repeat FNAB, if patients exhibit Tg-Ab positivity, no calcifications in nodules, and a DTD pattern on US.
MeSH Terms
-
Aged
Aged, 80 and over
Autoantibodies
Biopsy, Fine-Needle/*methods
Calcinosis
Carcinoma/*pathology
Female
Hashimoto Disease
Humans
Hyperplasia/*pathology
Male
Middle Aged
Multivariate Analysis
Predictive Value of Tests
Retrospective Studies
Sensitivity and Specificity
Thyroglobulin/blood
Thyroid Diseases
Thyroid Neoplasms/*pathology
Thyroid Nodule/*pathology
Thyroiditis, Autoimmune/*pathology
Thyrotropin/blood
Autoantibodies
Thyroglobulin
Thyrotropin
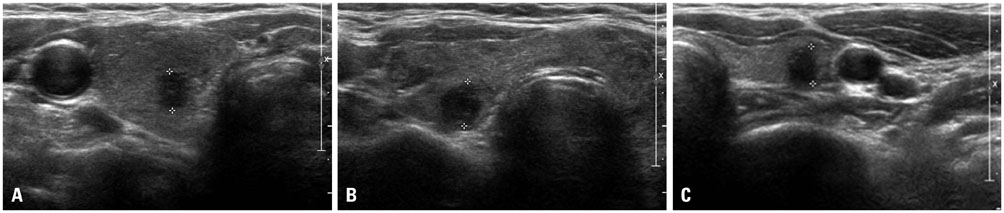
Figure
Cited by 3 articles
-
Changes of Nodular Size and Its Risk Factors in Iodine-Sufficient Area: a Retrospective Cohort Analysis of 7753 Thyroid Nodules
Hwa Young Ahn, Kyung Won Kim, Hoon Sung Choi, Jae Hoon Moon, Ka Hee Yi, Min Kyung Hyun, Min Joo Kang, Jung Im Shim, Ja Youn Lee, Do Joon Park, Young Joo Park
Int J Thyroidol. 2020;13(2):118-127. doi: 10.11106/ijt.2020.13.2.118.Thyroid nodules with discordant results of ultrasonographic and fine-needle aspiration findings
Min Joo Kim, Ka Hee Yi
J Korean Med Assoc. 2018;61(4):225-231. doi: 10.5124/jkma.2018.61.4.225.The Incidence and Clinicopathologic Characteristics of Patients Who Had False-Positive Fine-Needle Aspiration Results for Papillary Thyroid Cancer
Yoonju Bang, Kyorim Back, Jung-Han Kim, Junho Choe, Jee Soo Kim
J Endocr Surg. 2019;19(4):136-143. doi: 10.16956/jes.2019.19.4.136.
Reference
-
1. Mortensen JD, Woolner LB, Bennett WA. Gross and microscopic findings in clinically normal thyroid glands. J Clin Endocrinol Metab. 1955; 15:1270–1280.2. Singer PA. Evaluation and management of the solitary thyroid nodule. Otolaryngol Clin North Am. 1996; 29:577–591.3. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993; 328:553–559.4. Ross DS. Nonpalpable thyroid nodules--managing an epidemic. J Clin Endocrinol Metab. 2002; 87:1938–1940.5. Langer JE, Khan A, Nisenbaum HL, Baloch ZW, Horii SC, Coleman BG, et al. Sonographic appearance of focal thyroiditis. AJR Am J Roentgenol. 2001; 176:751–754.6. Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med. 2004; 351:1764–1771.7. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002; 178:687–691.
Article8. Peccin S, de Castsro JA, Furlanetto TW, Furtado AP, Brasil BA, Czepielewski MA. Ultrasonography: is it useful in the diagnosis of cancer in thyroid nodules? J Endocrinol Invest. 2002; 25:39–43.
Article9. Hegedüs L. Thyroid ultrasonography as a screening tool for thyroid disease. Thyroid. 2004; 14:879–880.
Article10. Ylagan LR, Farkas T, Dehner LP. Fine needle aspiration of the thyroid: a cytohistologic correlation and study of discrepant cases. Thyroid. 2004; 14:35–41.
Article11. Sangalli G, Serio G, Zampatti C, Bellotti M, Lomuscio G. Fine needle aspiration cytology of the thyroid: a comparison of 5469 cytological and final histological diagnoses. Cytopathology. 2006; 17:245–250.
Article12. Raab SS, Vrbin CM, Grzybicki DM, Sudilovsky D, Balassanian R, Zarbo RJ, et al. Errors in thyroid gland fine-needle aspiration. Am J Clin Pathol. 2006; 125:873–882.
Article13. Shin JH, Han BK, Ko K, Choe YH, Oh YL. Value of repeat ultrasound-guided fine-needle aspiration in nodules with benign cytological diagnosis. Acta Radiol. 2006; 47:469–473.
Article14. Chernyavsky VS, Shanker BA, Davidov T, Crystal JS, Eng O, Ibrahim K, et al. Is one benign fine needle aspiration enough? Ann Surg Oncol. 2012; 19:1472–1476.
Article15. Marcocci C, Vitti P, Cetani F, Catalano F, Concetti R, Pinchera A. Thyroid ultrasonography helps to identify patients with diffuse lymphocytic thyroiditis who are prone to develop hypothyroidism. J Clin Endocrinol Metab. 1991; 72:209–213.
Article16. Pedersen OM, Aardal NP, Larssen TB, Varhaug JE, Myking O, Vik-Mo H. The value of ultrasonography in predicting autoimmune thyroid disease. Thyroid. 2000; 10:251–259.17. Raber W, Gessl A, Nowotny P, Vierhapper H. Thyroid ultrasound versus antithyroid peroxidase antibody determination: a cohort study of four hundred fifty-one subjects. Thyroid. 2002; 12:725–731.18. Yeh HC, Futterweit W, Gilbert P. Micronodulation: ultrasonographic sign of Hashimoto thyroiditis. J Ultrasound Med. 1996; 15:813–819.
Article19. Takashima S, Matsuzuka F, Nagareda T, Tomiyama N, Kozuka T. Thyroid nodules associated with Hashimoto thyroiditis: assessment with US. Radiology. 1992; 185:125–130.
Article20. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.21. Cappelli C, Castellano M, Pirola I, Gandossi E, De Martino E, Cumetti D, et al. Thyroid nodule shape suggests malignancy. Eur J Endocrinol. 2006; 155:27–31.
Article22. Shin DY, Kim EK, Lee EJ. Role of ultrasonography in outcome prediction in subclinical hypothyroid patients treated with levothyroxine. Endocr J. 2010; 57:15–22.23. Nguyen GK, Lee MW, Ginsberg J, Wragg T, Bilodeau D. Fine-needle aspiration of the thyroid: an overview. Cytojournal. 2005; 2:12.24. Cappelli C, Pirola I, Cumetti D, Micheletti L, Tironi A, Gandossi E, et al. Is the anteroposterior and transverse diameter ratio of nonpalpable thyroid nodules a sonographic criteria for recommending fine-needle aspiration cytology? Clin Endocrinol (Oxf). 2005; 63:689–693.
Article25. Takashima S, Fukuda H, Nomura N, Kishimoto H, Kim T, Kobayashi T. Thyroid nodules: re-evaluation with ultrasound. J Clin Ultrasound. 1995; 23:179–184.26. Hayashi N, Tamaki N, Konishi J, Yonekura Y, Senda M, Kasagi K, et al. Sonography of Hashimoto's thyroiditis. J Clin Ultrasound. 1986; 14:123–126.
Article27. Bastin S, Bolland MJ, Croxson MS. Role of ultrasound in the assessment of nodular thyroid disease. J Med Imaging Radiat Oncol. 2009; 53:177–187.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphocytic Thyroiditis Presenting as a Focal Uptake on 18F-Fluorodeoxyglucose Positron Emission Tomography: A Case Report
- Ultrasonographic Findings of Papillary Thyroid Cancer with or without Hashimoto's Thyroiditis
- Lymphocytic Thyroiditis Presenting as Diffuse Microcalcifications on Ultrasound: A Case Report
- Sonographic Findings of Hashimoto's Thyroiditis and Associated Nodular Lesions
- Hashimoto's Thyroiditis and Coexistent Thyroid Cancer: Assessment with Sonography, Scintigraphy & CT