J Periodontal Implant Sci.
2016 Apr;46(2):72-83. 10.5051/jpis.2016.46.2.72.
Retrospective long-term analysis of bone level changes after horizontal alveolar crest reconstruction with autologous bone grafts harvested from the posterior region of the mandible
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Campus Virchow Clinic, Charité - Universitätsmedizin Berlin, Berlin, Germany. susanne.nahles@charite.de
- 2Dental Practice, Belleza-Praxisklinik für Implantologie und Ästhetik, Berlin, Germany.
- 3Department of Oral and Maxillofacial Surgery, Medical Center - University of Freiburg, Freiburg, Germany.
- KMID: 2161984
- DOI: http://doi.org/10.5051/jpis.2016.46.2.72
Abstract
- PURPOSE
The goal of this study was to evaluate the long-term success of horizontal alveolar crest augmentation of the retromolar region of the mandible with particulated bone, as well as factors affecting subsequent peri-implant bone loss.
METHODS
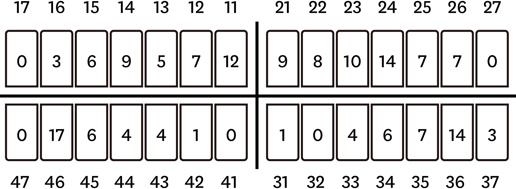
A total of 109 patients (68 female, 41 male) suffering from alveolar ridge deficiencies of the maxilla and mandible were included in this study. All patients were treated with particulated retromolar bone grafts from the mandible prior to the insertion of endosseous dental implants. Mesial and distal peri-implant crestal bone changes were assessed at six time points. Several parameters, including implant survival and the influence of age, gender, localisation of the implant, diameter, covering procedures, and time points of implant placement, were analysed to identify associations with bone level changes using the Mann-Whitney U-test, the Kruskal-Wallis test, and Spearman's rank-order correlation coefficient.
RESULTS
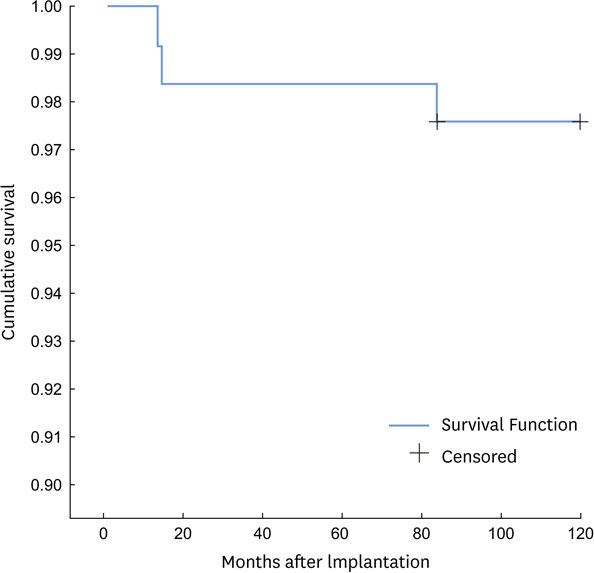
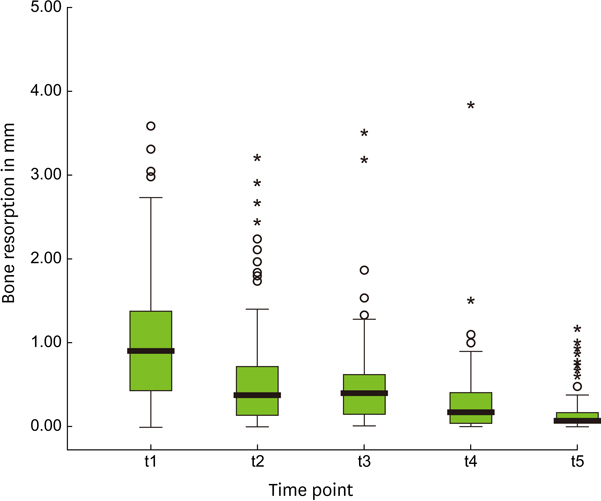
A total of 164 dental implants were placed in the maxilla (n=97) and in the mandible (n=67). The mean observation period was 105.26±21.58 months after implantation. The overall survival rate was 97.6% after 10 years. Overall, peri-implant bone loss was highest during the first year, but decreased over time. The mean amount of bone loss after 10 years was 2.47 mm mesially and 2.50 mm distally. Bone loss was significantly influenced by implant type and primary stability.
CONCLUSIONS
The use of particulated autologous retromolar bone grafts is a reliable technique for the horizontal reconstruction of local alveolar ridge deficiencies. Our results demonstrate that implants placed in augmented bone demonstrated similar bone level changes compared to implants inserted in non-augmented regions.
Keyword
MeSH Terms
Figure
Reference
-
1. Buser D, Dula K, Hess D, Hirt HP, Belser UC. Localized ridge augmentation with autografts and barrier membranes. Periodontol 2000. 1999; 19:151–163.
Article2. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007; 22:Suppl. 49–70.3. Al-Nawas B, Schiegnitz E. Augmentation procedures using bone substitute materials or autogenous bone - a systematic review and meta-analysis. Eur J Oral Implantology. 2014; 7:Suppl 2. S219–34.4. Pape HC, Evans A, Kobbe P. Autologous bone graft: properties and techniques. J Orthop Trauma. 2010; 24:Suppl 1. S36–40.
Article5. Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997; 12:767–776.6. Sittitavornwong S, Gutta R. Bone graft harvesting from regional sites. Oral Maxillofac Surg Clin North Am. 2010; 22:317–330. v–vi.
Article7. Chiapasco M, Zaniboni M, Boisco M. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res. 2006; 17:Suppl 2. 136–159.
Article8. Aloy-Prósper A, Maestre-Ferrin L, Peñarrocha-Oltra D, Peñarrocha-Diago M. Bone regeneration using particulate grafts: an update. Med Oral Patol Oral Cir Bucal. 2011; 16:e210–4.9. Dasmah A, Thor A, Ekestubbe A, Sennerby L, Rasmusson L. Particulate vs. block bone grafts: three-dimensional changes in graft volume after reconstruction of the atrophic maxilla, a 2-year radiographic follow-up. J Craniomaxillofac Surg. 2012; 40:654–659.
Article10. Ozaki W, Buchman SR. Volume maintenance of onlay bone grafts in the craniofacial skeleton: micro-architecture versus embryologic origin. Plast Reconstr Surg. 1998; 102:291–299.
Article11. Klijn RJ, Meijer GJ, Bronkhorst EM, Jansen JA. Sinus floor augmentation surgery using autologous bone grafts from various donor sites: a meta-analysis of the total bone volume. Tissue Eng Part B Rev. 2010; 16:295–303.
Article12. Nkenke E, Radespiel-Tröger M, Wiltfang J, Schultze-Mosgau S, Winkler G, Neukam FW. Morbidity of harvesting of retromolar bone grafts: a prospective study. Clin Oral Implants Res. 2002; 13:514–521.
Article13. Raghoebar GM, Meijndert L, Kalk WW, Vissink A. Morbidity of mandibular bone harvesting: a comparative study. Int J Oral Maxillofac Implants. 2007; 22:359–365.14. Clavero J, Lundgren S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res. 2003; 5:154–160.
Article15. Cordaro L, Torsello F, Miuccio MT, di Torresanto VM, Eliopoulos D. Mandibular bone harvesting for alveolar reconstruction and implant placement: subjective and objective cross-sectional evaluation of donor and recipient site up to 4 years. Clin Oral Implants Res. 2011; 22:1320–1326.
Article16. Misch CE. Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol. 1990; 6:23–31.17. Semper W, Heberer S, Nelson K. Retrospective analysis of bar-retained dentures with cantilever extension: marginal bone level changes around dental implants over time. Int J Oral Maxillofac Implants. 2010; 25:385–393.18. Gomez-Roman G, Schulte W, d’Hoedt B, Axman-Krcmar D. The Frialit-2 implant system: five-year clinical experience in single-tooth and immediately postextraction applications. Int J Oral Maxillofac Implants. 1997; 12:299–309.19. Louis PJ, Gutta R, Said-Al-Naief N, Bartolucci AA. Reconstruction of the maxilla and mandible with particulate bone graft and titanium mesh for implant placement. J Oral Maxillofac Surg. 2008; 66:235–245.
Article20. Simion M, Fontana F, Rasperini G, Maiorana C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin Oral Implants Res. 2007; 18:620–629.
Article21. Trombelli L, Farina R, Marzola A, Itro A, Calura G. GBR and autogenous cortical bone particulate by bone scraper for alveolar ridge augmentation: a 2-case report. Int J Oral Maxillofac Implants. 2008; 23:111–116.22. Moraschini V, Poubel LA, Ferreira VF, Barboza ES. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015; 44:377–388.
Article23. Tinsley D, Watson CJ, Ogden AR. A survey of U.K. centres on implant failures. J Oral Rehabil. 1999; 26:14–18.
Article24. Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977; 16:1–132.25. Verhoeven JW, Cune MS, Terlou M, Zoon MA, de Putter C. The combined use of endosteal implants and iliac crest onlay grafts in the severely atrophic mandible: a longitudinal study. Int J Oral Maxillofac Surg. 1997; 26:351–357.
Article26. Duttenhoefer F, Nack C, Doll C, Raguse JD, Hell B, Stricker A, et al. Long-term peri-implant bone level changes of non-vascularized fibula bone grafted edentulous patients. J Craniomaxillofac Surg. 2015; 43:611–615.
Article27. Fretwurst T, Nack C, Al-Ghrairi M, Raguse JD, Stricker A, Schmelzeisen R, et al. Long-term retrospective evaluation of the peri-implant bone level in onlay grafted patients with iliac bone from the anterior superior iliac crest. J Craniomaxillofac Surg. 2015; 43:956–960.
Article28. Peñarrocha-Oltra D, Aloy-Prósper A, Cervera-Ballester J, Peñarrocha-Diago M, Canullo L, Peñarrocha-Diago M. Implant treatment in atrophic posterior mandibles: vertical regeneration with block bone grafts versus implants with 5.5-mm intrabony length. Int J Oral Maxillofac Implants. 2014; 29:659–666.
Article29. Chiapasco M, Casentini P, Zaniboni M, Corsi E. Evaluation of peri-implant bone resorption around Straumann Bone Level implants placed in areas reconstructed with autogenous vertical onlay bone grafts. Clin Oral Implants Res. 2012; 23:1012–1021.
Article30. Hartman GA, Cochran DL. Initial implant position determines the magnitude of crestal bone remodeling. J Periodontol. 2004; 75:572–577.
Article31. Jones AA, Cochran DL. Consequences of implant design. Dent Clin North Am. 2006; 50:339–360. v
Article32. Ozaki W, Buchman SR, Goldstein SA, Fyhrie DP. A comparative analysis of the microarchitecture of cortical membranous and cortical endochondral onlay bone grafts in the craniofacial skeleton. Plast Reconstr Surg. 1999; 104:139–147.
Article33. Sugg KB, Rosenthal AH, Ozaki W, Buchman SR. Quantitative comparison of volume maintenance between inlay and onlay bone grafts in the craniofacial skeleton. Plast Reconstr Surg. 2013; 131:1014–1021.
Article34. Fonseca RJ, Nelson JF, Clark PJ, Frost DE, Olson RA. Revascularization and healing of onlay particulate allogeneic bone grafts in primates. J Oral Maxillofac Surg. 1983; 41:153–162.
Article35. Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010; 38:612–620.
Article36. Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006; 17:244–250.
Article37. Clementini M, Morlupi A, Agrestini C, Barlattani A. Immediate versus delayed positioning of dental implants in guided bone regeneration or onlay graft regenerated areas: a systematic review. Int J Oral Maxillofac Surg. 2013; 42:643–650.
Article38. Strietzel FP, Khongkhunthian P, Khattiya R, Patchanee P, Reichart PA. Healing pattern of bone defects covered by different membrane types--a histologic study in the porcine mandible. J Biomed Mater Res B Appl Biomater. 2006; 78:35–46.
Article39. Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Küchler I. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007; 34:523–544.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Horizontal ridge augmentation with porcine bone-derived grafting material: a long-term retrospective clinical study with more than 5 years of follow-up
- Reconstruction of alveolar clefts with iliac cancellous particulate or block bone grafts: a comparative study
- The Reharvesting of Iliac Crest Cancellous Bone for the Repair of the Alveolar Cleft
- Eruption of a venous malformation through an iliac bone harvesting site after trauma
- The preliminary study for three-dimensional alveolar bone morphologic characteristics for alveolar bone restoration