J Korean Soc Radiol.
2015 Mar;72(3):202-205. 10.3348/jksr.2015.72.3.202.
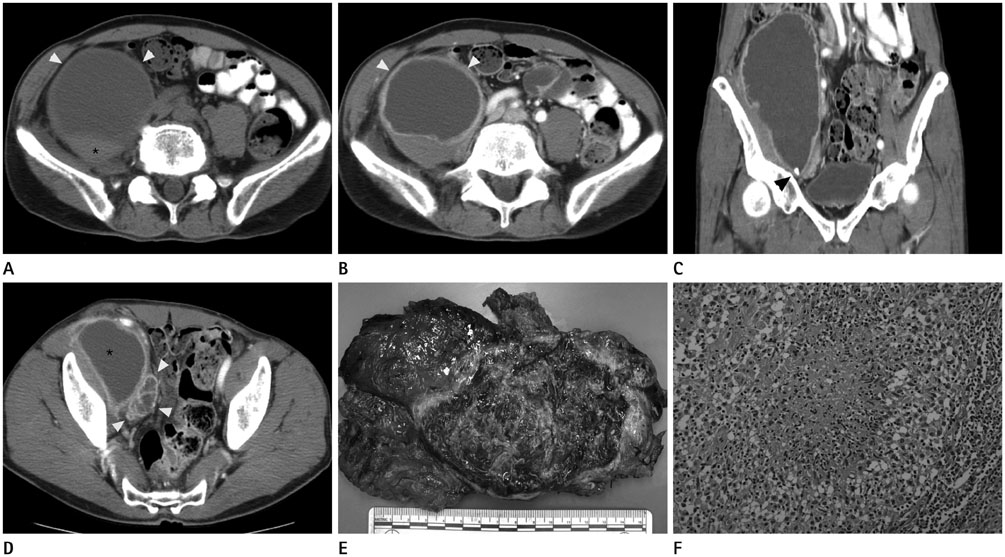
A Large Tuberculous Abscess Mimicking a Retroperitoneal Cystic Mass: A Case Report
- Affiliations
-
- 1Department of Radiology, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea. peace22@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea.
- KMID: 2161175
- DOI: http://doi.org/10.3348/jksr.2015.72.3.202
Abstract
- Large cystic masses originating from the retroperitoneal space are rare, and cystic tumors are often considered preferentially in the differential diagnosis. However, it is difficult to make a correct diagnosis. A 55-year-old man presented with a palpable abdominal mass. A computed tomography (CT) scan detected a mass mimicking a large cystic tumor in the retroperitoneal space anterior to the psoas muscle. The mass had an enhanced outer margin, an irregular inner margin, and several surrounding necrotic lymph nodes. However, histopathologic examination followed by an exploratory laparotomy confirmed that the mass was consistent with a tuberculous (TB) abscess. A retroperitoneal TB abscess without spinal or active pulmonary TB is very rare. To the best of our knowledge, there are no published reports of a retroperitoneal TB abscess confirmed by both CT scan and surgical pathology in the Korean literature. We report a rare case of a huge retroperitoneal TB abscess that can mimic a cystic tumor.
MeSH Terms
Figure
Reference
-
1. Kwon YS, Koh WJ. Diagnosis of pulmonary tuberculosis and nontuberculous mycobacterial lung disease in Korea. Tuberc Respir Dis. 2014; 77:1–5.2. Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005; 72:1761–1768.3. Barbalinardo RJ, Hamilton GB, Eliot GR, Lazaro EJ, Haycock C. Tuberculous retroperitoneal lymphadenopathy mimicking metastatic pancreatic carcinoma. J Natl Med Assoc. 1986; 78:385–387.4. Karoui S, Bibani N, Ouaz A, Serghini M, Chebbi F, Nouira K, et al. Retroperitoneal abscess: a rare localization of tubercular infection. Gastroenterol Res Pract. 2010; 2010:475130.5. Epstein BM, Mann JH. CT of abdominal tuberculosis. AJR Am J Roentgenol. 1982; 139:861–866.6. Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004; 24:1353–1365.7. Shin YS, Kim HJ, Kim MK. Juxta-adrenal malignant schwannoma with lymph node metastases. Can Urol Assoc J. 2013; 7:E657–E659.8. Fong Y, Coit DG, Woodruff JM, Brennan MF. Lymph node metastasis from soft tissue sarcoma in adults. Analysis of data from a prospective database of 1772 sarcoma patients. Ann Surg. 1993; 217:72–77.9. Chuang HJ, Liu JY, Chang FW, Chou CC, Loh CH. Vertebral tuberculosis presenting as a large retroperitoneal cyst. Taiwan J Obstet Gynecol. 2008; 47:247–249.10. Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004; 80:459–462.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retroperitoneal Cystic Lymphangioma with Change of Internal Morphology on Follow-up Ultrasound and CT: A Case Report
- A Case of Tuberculous Abscess in Cerebrum
- Cystic Change in a Primary Retroperitoneal Angiosarcoma: A Case Report
- A Case of Tuberculous Cerebellar Abscess: Case Report
- Retroperitoneal Abscess in a Patient with Acute Appendicitis