J Cardiovasc Ultrasound.
2016 Mar;24(1):64-67. 10.4250/jcu.2016.24.1.64.
Abnormal Myocardial Blood Flow Reserve Observed in Cardiac Amyloidosis
- Affiliations
-
- 1Department of Cardiology, Sunshine Coast Hospital and Health Service, Nambour, QLD, Australia. dr.michael.nam@gmail.com
- 2Department of Cardiology, Royal Brompton and Harefield NHS Trust, London, United Kingdom.
- KMID: 2160998
- DOI: http://doi.org/10.4250/jcu.2016.24.1.64
Abstract
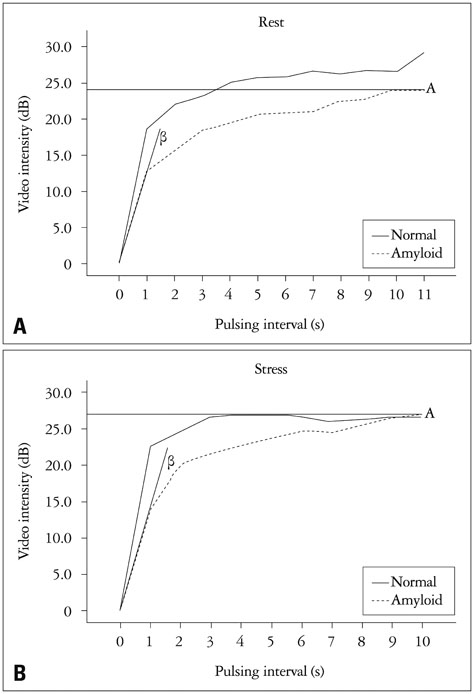
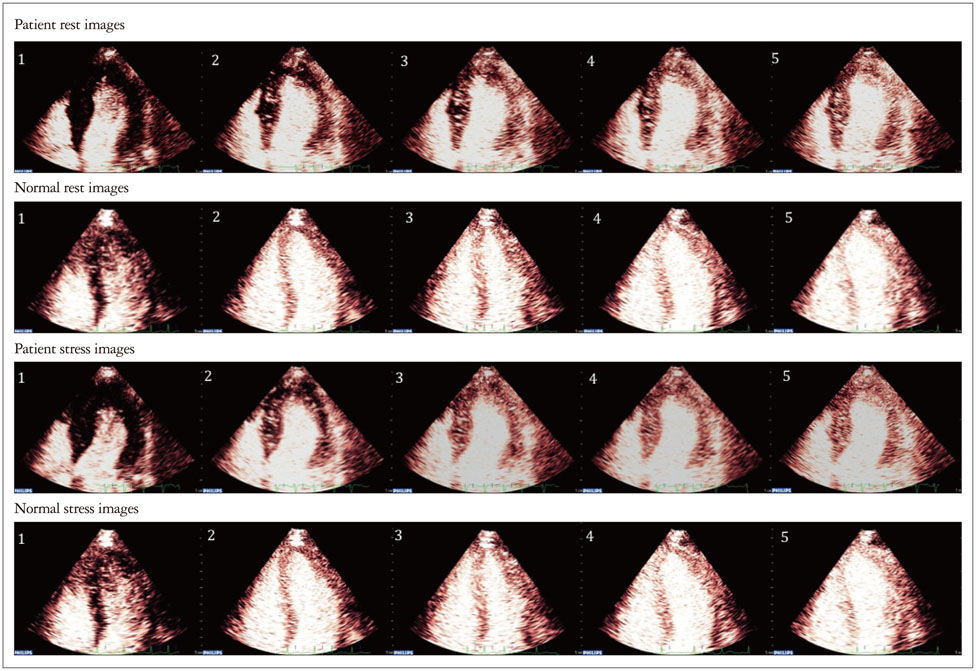
- We performed real-time myocardial contrast echocardiography on a patient with cardiac amyloidosis and previous normal coronary angiography presenting with atypical chest pain to assess myocardial blood flow reserve (MBFR). Myocardial contrast echocardiography was performed and flash microbubble destruction and replenishment analysis was used to calculate myocardial blood flow. Dipyridamole was used to achieve hyperemia. MBFR was derived from the ratio of peak myocardial blood flow at hyperemia and rest. The results show a marked reduction in MBFR in our patient. Previous reports of luminal obstruction of intramyocardial rather than epicardial vessels by amyloid deposition may be causing microvascular dysfunction.
Keyword
MeSH Terms
Figure
Reference
-
1. Narang R, Chopra P, Wasir HS. Cardiac amyloidosis presenting as ischemic heart disease. A case report and review of literature. Cardiology. 1993; 82:294–300.2. Neben-Wittich MA, Wittich CM, Mueller PS, Larson DR, Gertz MA, Edwards WD. Obstructive intramural coronary amyloidosis and myocardial ischemia are common in primary amyloidosis. Am J Med. 2005; 118:1287.3. Vogelsberg H, Mahrholdt H, Deluigi CC, Yilmaz A, Kispert EM, Greulich S, Klingel K, Kandolf R, Sechtem U. Cardiovascular magnetic resonance in clinically suspected cardiac amyloidosis: noninvasive imaging compared to endomyocardial biopsy. J Am Coll Cardiol. 2008; 51:1022–1030.4. Wei K, Ragosta M, Thorpe J, Coggins M, Moos S, Kaul S. Noninvasive quantification of coronary blood flow reserve in humans using myocardial contrast echocardiography. Circulation. 2001; 103:2560–2565.5. Rana O, Byrne CD, Kerr D, Coppini DV, Zouwail S, Senior R, Begley J, Walker JJ, Greaves K. Acute hypoglycemia decreases myocardial blood flow reserve in patients with type 1 diabetes mellitus and in healthy humans. Circulation. 2011; 124:1548–1556.6. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007; 356:830–840.7. Mueller PS, Edwards WD, Gertz MA. Symptomatic ischemic heart disease resulting from obstructive intramural coronary amyloidosis. Am J Med. 2000; 109:181–188.8. Apridonidze T, Steingart RM, Comenzo RL, Hoffman J, Goldsmith Y, Bella JN, Landau H, Liu JE. Clinical and echocardiographic correlates of elevated troponin in amyloid light-chain cardiac amyloidosis. Am J Cardiol. 2012; 110:1180–1184.9. Senior R, Becher H, Monaghan M, Agati L, Zamorano J, Vanoverschelde JL, Nihoyannopoulos P. Contrast echocardiography: evidencebased recommendations by European Association of Echocardiography. Eur J Echocardiogr. 2009; 10:194–212.10. Al Suwaidi J, Velianou JL, Gertz MA, Cannon RO 3rd, Higano ST, Holmes DR Jr, Lerman A. Systemic amyloidosis presenting with angina pectoris. Ann Intern Med. 1999; 131:838–841.11. Abdelmoneim SS, Bernier M, Bellavia D, Syed IS, Mankad SV, Chandrasekaran K, Pellikka PA, Mulvagh SL. Myocardial contrast echocardiography in biopsy-proven primary cardiac amyloidosis. Eur J Echocardiogr. 2008; 9:338–341.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Myocardial Blood Flow and Coronary Flow Reserve Using Positron Emission Tomography
- Myocardial fractional flow reserve in acute myocardial infarction
- Myocardial Contrast Echocardiography for the Assessment of Coronary Blood Flow Reserve
- Coronary Flow Velocity Pattern in Patients with Myocardial Bridging of Coronary Artery
- Contemporary Imaging Diagnosis of Cardiac Amyloidosis