Korean J Radiol.
2015 Oct;16(5):1012-1023. 10.3348/kjr.2015.16.5.1012.
Measurement of Opening and Closing Angles of Aortic Valve Prostheses In Vivo Using Dual-Source Computed Tomography: Comparison with Those of Manufacturers' in 10 Different Types
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul 03722, Korea. dryj@yuhs.ac
- KMID: 2160768
- DOI: http://doi.org/10.3348/kjr.2015.16.5.1012
Abstract
OBJECTIVE
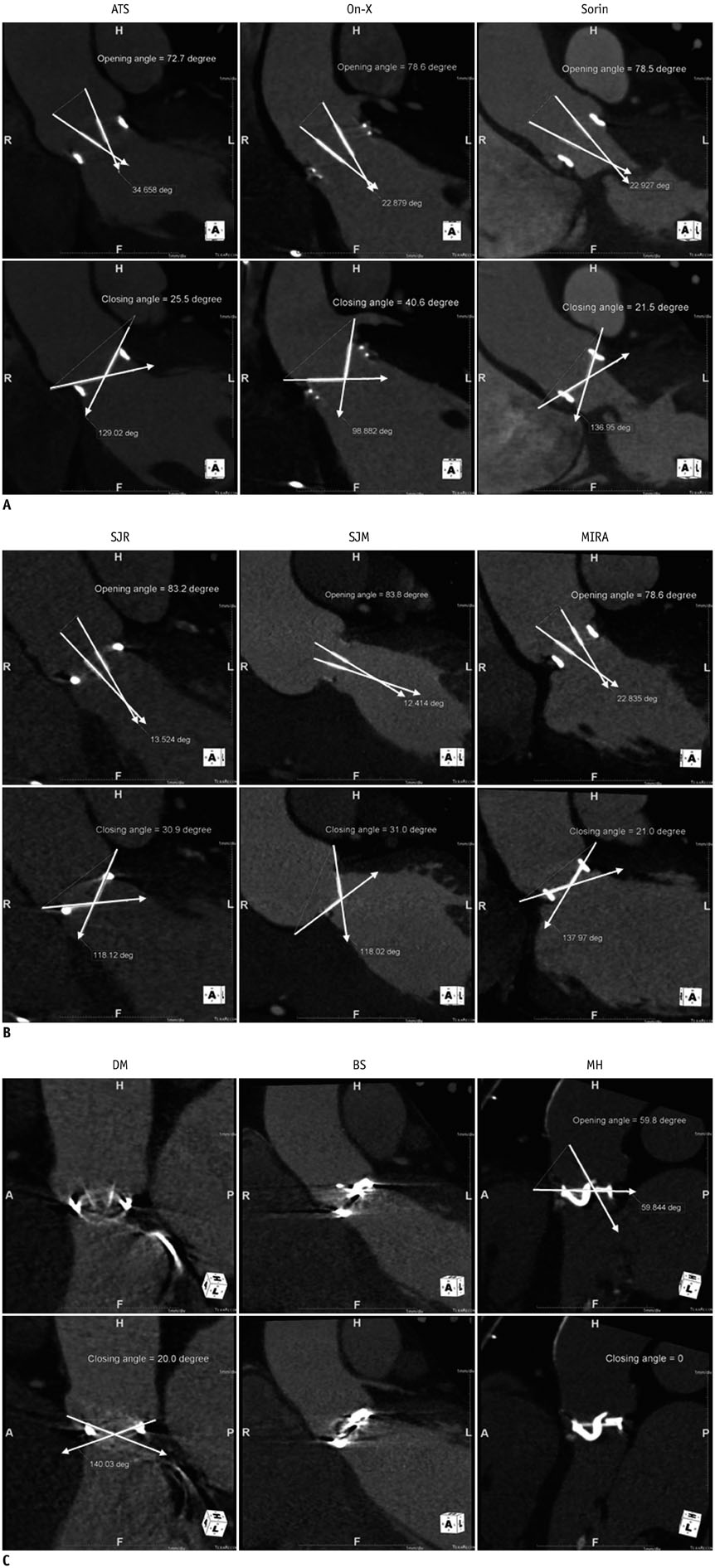
The aims of this study were to compare opening and closing angles of normally functioning mechanical aortic valves measured on dual-source computed tomography (CT) with the manufacturers' values and to compare CT-measured opening angles according to valve function.
MATERIALS AND METHODS
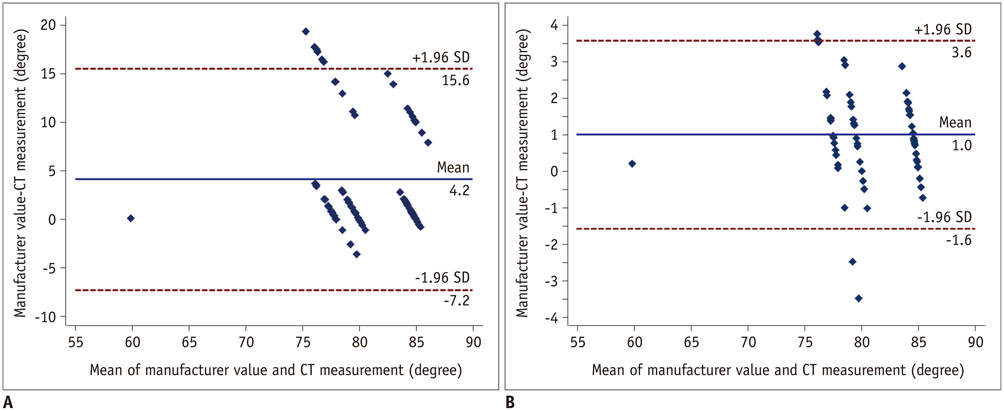
A total of 140 patients with 10 different types of mechanical aortic valves, who underwent dual-source cardiac CT, were included. Opening and closing angles were measured on CT images. Agreement between angles in normally functioning valves and the manufacturer values was assessed using the interclass coefficient and the Bland-Altman method. CT-measured opening angles were compared between normal functioning valves and suspected dysfunctioning valves.
RESULTS
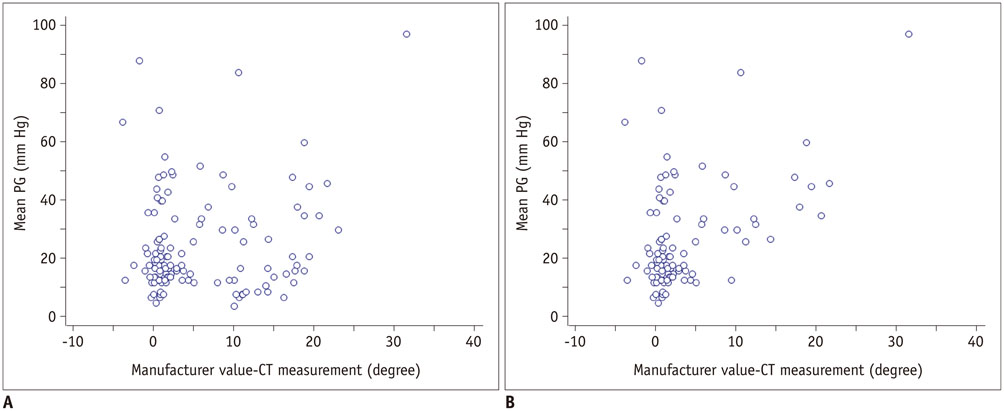
The CT-measured opening angles of normally functioning valves and manufacturers' values showed excellent agreement for seven valve types (intraclass coefficient [ICC], 0.977; 95% confidence interval [CI], 0.962-0.987). The mean differences in opening angles between the CT measurements and the manufacturers' values were 1.2degrees in seven types of valves, 11.0degrees in On-X valves, and 15.5degrees in ATS valves. The manufacturers' closing angles and those measured by CT showed excellent agreement for all valve types (ICC, 0.953; 95% CI, 0.920-0.972). Among valves with suspected dysfunction, those with limitation of motion (LOM) and an increased pressure gradient (PG) had smaller opening angles than those with LOM only (p < 0.05).
CONCLUSION
Dual-source cardiac CT accurately measures opening and closing angles in most types of mechanical aortic valves, compared with the manufacturers' values. Opening angles on CT differ according to the type of valve dysfunction and a decreased opening angle may suggest an elevated PG.
Keyword
MeSH Terms
Figure
Reference
-
1. Bach DS. Echo/Doppler evaluation of hemodynamics after aortic valve replacement: principles of interrogation and evaluation of high gradients. JACC Cardiovasc Imaging. 2010; 3:296–304.2. Carrier M, Pellerin M, Basmadjian A, Bouchard D, Perrault LP, Cartier R, et al. Fifteen years of clinical and echocardiographic follow up with the carbomedics heart valve. J Heart Valve Dis. 2006; 15:67–72. discussion 723. LaBounty TM, Agarwal PP, Chughtai A, Bach DS, Wizauer E, Kazerooni EA. Evaluation of mechanical heart valve size and function with ECG-gated 64-MDCT. AJR Am J Roentgenol. 2009; 193:W389–W396.4. Konen E, Goitein O, Feinberg MS, Eshet Y, Raanani E, Rimon U, et al. The role of ECG-gated MDCT in the evaluation of aortic and mitral mechanical valves: initial experience. AJR Am J Roentgenol. 2008; 191:26–31.5. Lee DH, Youn HJ, Shim SB, Lee SH, Jung JI, Jung SE, et al. The measurement of opening angle and orifice area of a bileaflet mechanical valve using multidetector computed tomography. Korean Circ J. 2009; 39:157–162.6. Suchá D, Symersky P, Vonken EJ, Provoost E, Chamuleau SA, Budde RP. Multidetector-row computed tomography allows accurate measurement of mechanical prosthetic heart valve leaflet closing angles compared with fluoroscopy. J Comput Assist Tomogr. 2014; 38:451–456.7. Tsai IC, Lin YK, Chang Y, Fu YC, Wang CC, Hsieh SR, et al. Correctness of multi-detector-row computed tomography for diagnosing mechanical prosthetic heart valve disorders using operative findings as a gold standard. Eur Radiol. 2009; 19:857–867.8. Teshima H, Hayashida N, Fukunaga S, Tayama E, Kawara T, Aoyagi S, et al. Usefulness of a multidetector-row computed tomography scanner for detecting pannus formation. Ann Thorac Surg. 2004; 77:523–526.9. Ueda T, Teshima H, Fukunaga S, Aoyagi S, Tanaka H. Evaluation of prosthetic valve obstruction on electrocardiographically gated multidetector-row computed tomography--identification of subprosthetic pannus in the aortic position. Circ J. 2013; 77:418–423.10. Park YJ, Kim YJ, Lee JW, Kim HY, Hong YJ, Lee HJ, et al. Automatic Tube Potential Selection with Tube Current Modulation (APSCM) in coronary CT angiography: Comparison of image quality and radiation dose with conventional body mass index-based protocol. J Cardiovasc Comput Tomogr. 2012; 6:184–190.11. Suh YJ, Kim YJ, Hong SR, Hong YJ, Lee HJ, Hur J, et al. Combined use of automatic tube potential selection with tube current modulation and iterative reconstruction technique in coronary CT angiography. Radiology. 2013; 269:722–729.12. Symersky P, Budde RP, de Mol BA, Prokop M. Comparison of multidetector-row computed tomography to echocardiography and fluoroscopy for evaluation of patients with mechanical prosthetic valve obstruction. Am J Cardiol. 2009; 104:1128–1134.13. Aoyagi S, Arinaga K, Fukunaga S, Tayama E, Kosuga T, Akashi H. Leaflet movement of the ATS valve in the aortic position: unique behavior observed in 19-mm valves. Ann Thorac Surg. 2006; 82:853–857.14. Feng Z, Nakamura T, Fujimoto T, Umezu M. In vitro investigation of opening behavior and hydrodynamics of bileaflet valves in the mitral position. Artif Organs. 2002; 26:32–39.15. Parnell A, Swanevelder J. High transvalvular pressure gradients on intraoperative transesophageal echocardiography after aortic valve replacement: what does it mean? HSR Proc Intensive Care Cardiovasc Anesth. 2009; 1:7–18.16. Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA, et al. Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report From the American Society of Echocardiography's Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2009; 22:975–1014. quiz 1082-108417. Tayama E, Feng Z, Oda T, Tomoeda H, Hayashida N, Fukunaga S, et al. ATS prosthetic valve motion: an in vitro analysis. J Heart Valve Dis. 2000; 9:408–414.18. Habets J, Mali WP, Budde RP. Multidetector CT angiography in evaluation of prosthetic heart valve dysfunction. Radiographics. 2012; 32:1893–1905.19. Habets J, Budde RP, Symersky P, van den Brink RB, de Mol BA, Mali WP, et al. Diagnostic evaluation of left-sided prosthetic heart valve dysfunction. Nat Rev Cardiol. 2011; 8:466–478.20. Montorsi P, Arena V, Muratori M, Lavarra F, Cavoretto D, Repossini A, et al. Fluoroscopic functional evaluation of bileaflet prostheses: effect of different intraoperative valve orientation. Am J Card Imaging. 1996; 10:101–107.21. Cianciulli TE, Lax JA, Beck MA, Cerruti FE, Gigena GE, Saccheri MC, et al. Cinefluoroscopic assessment of mechanical disc prostheses: its value as a complementary method to echocardiography. J Heart Valve Dis. 2005; 14:664–673.22. Cianciulli TF, Saccheri MC, Lax JA, Guidoin R, Zhang Z, Guerra JE, et al. Intermittent acute aortic regurgitation of a mechanical bileaflet aortic valve prosthesis: diagnosis and clinical implications. Eur J Echocardiogr. 2009; 10:446–449.23. Kuniyoshi Y, Koja K, Miyagi K, Shimoji M, Uezu T, Arakaki K, et al. Pannus formation in aortic valve prostheses in the late postoperative period. J Artif Organs. 2003; 6:179–182.24. Teshima H, Hayashida N, Yano H, Nishimi M, Tayama E, Fukunaga S, et al. Obstruction of St Jude Medical valves in the aortic position: histology and immunohistochemistry of pannus. J Thorac Cardiovasc Surg. 2003; 126:401–407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Measurement of Opening Angle and Orifice Area of a Bileaflet Mechanical Valve Using Multidetector Computed Tomography
- Expanding transcatheter aortic valve replacement into uncharted indications
- Quadricuspid Aortic Valve : Report of Three Cases and Review of the Literature
- Echocardiographic Characteristics of Normally Functioning CarboMedics and St.Jude Medical Mitral Valve
- Aortic Valve Repair