J Korean Med Sci.
2015 Jun;30(6):763-769. 10.3346/jkms.2015.30.6.763.
Relationship between the Clinical Characteristics and Intervention Scores of Infants with Apparent Life-threatening Events
- Affiliations
-
- 1Department of Pediatrics, Keimyung University School of Medicine, Daegu, Korea.
- 2Department of Pediatrics, Kyungpook National University School of Medicine, Daegu, Korea. kimyhmd@knu.ac.kr
- KMID: 2160606
- DOI: http://doi.org/10.3346/jkms.2015.30.6.763
Abstract
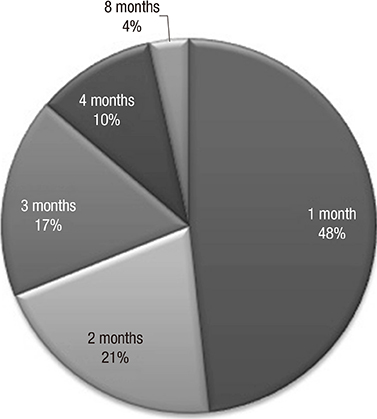
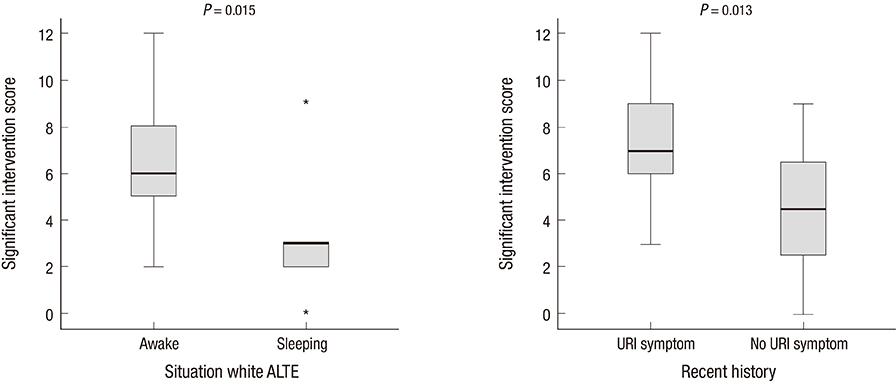
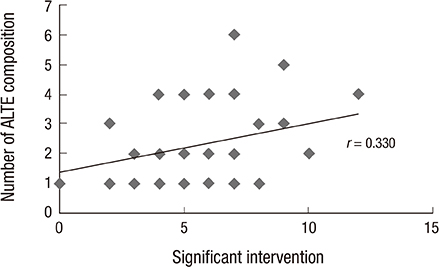
- We investigated the clinical presentations, diagnostic and therapeutic modalities, and prognosis from follow-up of infants with apparent life-threatening events (ALTE). In addition, the relationship between the clinical characteristics of patients and significant intervention scores was analyzed. We enrolled patients younger than 12 months who were diagnosed with ALTE from January 2005 to December 2012. There were 29 ALTE infants with a peak incidence of age younger than 1 month (48.3%). The most common symptoms for ALTE diagnosis were apnea (69.0%) and color change (58.6%). Eleven patients appeared normal upon arrival at hospital but 2 patients required cardiopulmonary resuscitation during the initial ALTE. The most common ALTE cause was respiratory disease, including respiratory infection and upper airway anomalies (44.8%). There were 20 cases of repeat ALTE and 2 cases of death during hospitalization. Four patients (15.4%) experienced recurrence of ALTE after discharge and 4 patients (15.4%) showed developmental abnormalities during the follow-up period. The patients with ALTE during sleep had lower significant intervention scores (P=0.015) compared to patients with ALTE during wakefulness and patients with previous respiratory symptoms had higher significant intervention scores (P=0.013) than those without previous respiratory symptoms. Although not statistically significant, there was a weak positive correlation between the patient's total ALTE criteria and total significant intervention score (Fig. 2, r=0.330, P=0.080). We recommend that all ALTE infants undergo inpatient observation and evaluations with at least 24 hr of cardiorespiratory monitoring, and should follow up at least within a month after discharge.
MeSH Terms
-
Age Distribution
Clinical Decision-Making
Critical Care/*statistics & numerical data
Critical Illness/*mortality/*therapy
Female
*Hospital Mortality
Hospitalization/*statistics & numerical data
Humans
Incidence
Infant
Infant, Newborn
Male
Republic of Korea/epidemiology
Risk Factors
Sex Distribution
Survival Rate
Treatment Outcome
Figure
Reference
-
1. American Academy. Task Force on Prolonged Infantile Apnea. Prolonged infantile apnea: 1985. Pediatrics. 1985; 76:129–131.2. National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, Sept 29 to Oct 1, 1986. Pediatrics. 1987; 79:292–299.3. Gray C, Davies F, Molyneux E. Apparent life-threatening events presenting to a pediatric emergency department. Pediatr Emerg Care. 1999; 15:195–199.4. Davies F, Gupta R. Apparent life threatening events in infants presenting to an emergency department. Emerg Med J. 2002; 19:11–16.5. Mittal MK, Shofer FS, Baren JM. Serious bacterial infections in infants who have experienced an apparent life-threatening event. Ann Emerg Med. 2009; 54:523–527.6. Shah S, Sharieff GQ. An update on the approach to apparent life-threatening events. Curr Opin Pediatr. 2007; 19:288–294.7. Oren J, Kelly D, Shannon DC. Identification of a high-risk group for sudden infant death syndrome among infants who were resuscitated for sleep apnea. Pediatrics. 1986; 77:495–499.8. Committee on Fetus and Newborn. American Academy of Pediatrics. Apnea, sudden infant death syndrome, and home monitoring. Pediatrics. 2003; 111:914–917.9. De Piero AD, Teach SJ, Chamberlain JM. ED evaluation of infants after an apparent life-threatening event. Am J Emerg Med. 2004; 22:83–86.10. Claudius I, Keens T. Do all infants with apparent life-threatening events need to be admitted? Pediatrics. 2007; 119:679–683.11. Al-Kindy HA, Gélinas JF, Hatzakis G, Côté AC. Risk factors for extreme events in infants hospitalized for apparent life-threatening events. J Pediatr. 2009; 154:332–337. 337.e1–337.e2.12. Mittal MK, Sun G, Baren JM. A clinical decision rule to identify infants with apparent life-threatening event who can be safely discharged from the emergency department. Pediatr Emerg Care. 2012; 28:599–605.13. Kahn A. European Society for the Study and Prevention of Infant Death. Recommended clinical evaluation of infants with an apparent life-threatening event. Consensus document of the European Society for the Study and Prevention of Infant Death, 2003. Eur J Pediatr. 2004; 163:108–115.14. Kahn A, Rebuffat E, Franco P, N'Duwimana M, Blum D. Apparent life-threatening events and apnea of infancy. In : Beckerman RC, Brouillette RT, Hunt CE, editors. Respiratory control disorders in infants and children. Baltimore: Williams & Wilkins;1992. p. 178–189.15. Al Khushi N, Côté A. Apparent life-threatening events: assessment, risks, reality. Paediatr Respir Rev. 2011; 12:124–132.16. Brand DA, Altman RL, Purtill K, Edwards KS. Yield of diagnostic testing in infants who have had an apparent life-threatening event. Pediatrics. 2005; 115:885–893.17. Altman RL, Li KI, Brand DA. Infections and apparent life-threatening events. Clin Pediatr (Phila). 2008; 47:372–378.18. Semmekrot BA, van Sleuwen BE, Engelberts AC, Joosten KF, Mulder JC, Liem KD, Rodrigues Pereira R, Bijlmer RP, L'Hoir MP. Surveillance study of apparent life-threatening events (ALTE) in the Netherlands. Eur J Pediatr. 2010; 169:229–236.19. Crowcroft NS, Zambon M, Harrison TG, Mok Q, Heath P, Miller E. Respiratory syncytial virus infection in infants admitted to paediatric intensive care units in London, and in their families. Eur J Pediatr. 2008; 167:395–399.20. Tieder JS, Altman RL, Bonkowsky JL, Brand DA, Claudius I, Cunningham DJ, DeWolfe C, Percelay JM, Pitetti RD, Smith MB. Management of apparent life-threatening events in infants: a systematic review. J Pediatr. 2013; 163:94–99.e1-6.21. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, Sondheimer J, Staiano A, Thomson M, Veereman-Wauters G, et al. North American Society for Pediatric Gastroenterology Hepatology and Nutrition, European Society for Pediatric Gastroenterology Hepatology and Nutrition. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.22. Bonkowsky JL, Guenther E, Filloux FM, Srivastava R. Death, child abuse, and adverse neurological outcome of infants after an apparent life-threatening event. Pediatrics. 2008; 122:125–131.23. Parker K, Pitetti R. Mortality and child abuse in children presenting with apparent life-threatening events. Pediatr Emerg Care. 2011; 27:591–595.24. Kant S, Fisher JD, Nelson DG, Khan S. Mortality after discharge in clinically stable infants admitted with a first-time apparent life-threatening event. Am J Emerg Med. 2013; 31:730–733.25. Nunes ML, Costa JC, Ferreira CP, Garcia CC, Marques FC, Spolidoro JV. Associated and prognosis in apparent life threatening events (ALTE). J Pediatr (Rio J). 1999; 75:55–58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Apparent life-threatening event in infancy
- Clinical Feature and General Management of Post-Hemorrhagic Hydrocephalus in Premature Infants
- Quality of Life in Patients with Psoriasis
- Quality of Life in Patients with Panic Disorder
- A Study on the Correlation among Family Life Events Stress, Family Functioning and Social Support of the Wives who Reside in Some Area