J Korean Foot Ankle Soc.
2016 Mar;20(1):39-42. 10.14193/jkfas.2016.20.1.39.
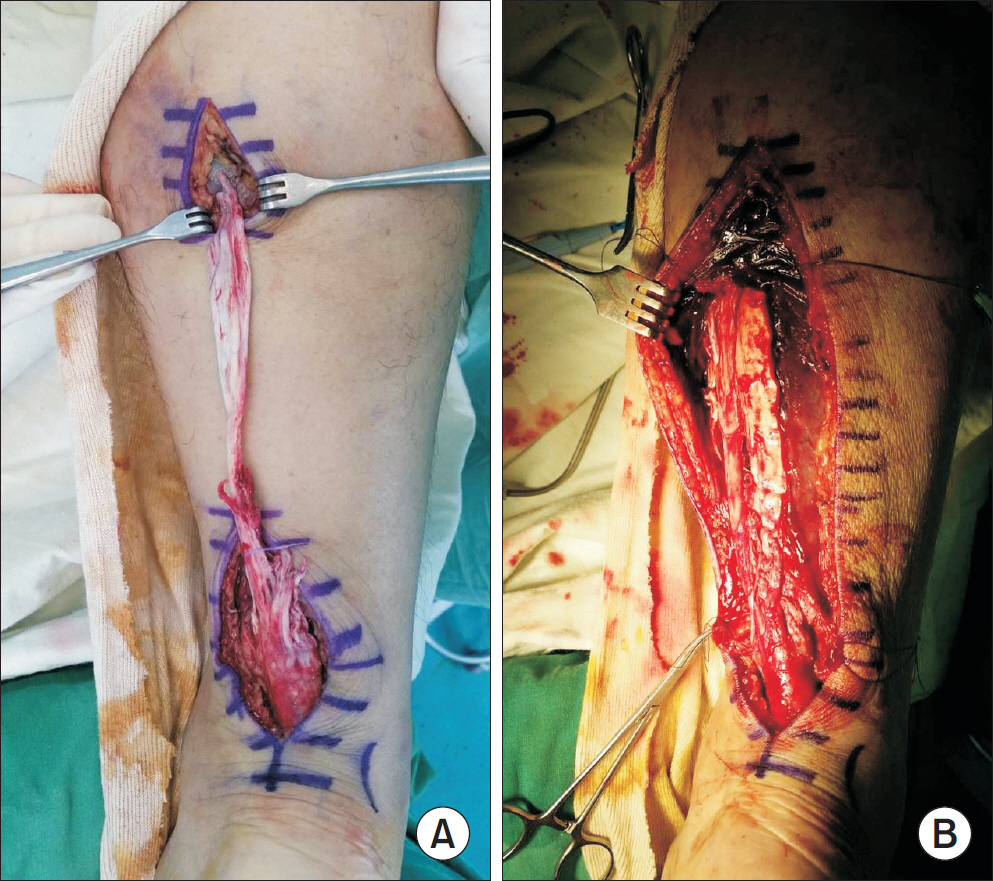
Deep Vein Thrombosis after Achilles Tendon Repair: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Dankook University College of Medicine, Cheonan, Korea. m3artist@hanmail.net
- KMID: 2158428
- DOI: http://doi.org/10.14193/jkfas.2016.20.1.39
Abstract
- Achilles tendon rupture is thought to be increasing with participation in sports activities. Both operative and non-operative treatments of Achilles tendon rupture include a period of immobilization. Complications following treatment of the Achilles tendon rupture include recurrence of rupture, flexor weakness, infection, and wound problems. However, deep vein thrombosis (DVT) after operative treatment of the Achilles tendon has not been reported. We report on a case of DVT after Achilles tendon repair.
MeSH Terms
Figure
Reference
-
References
1. Lapidus LJ, Rosfors S, Ponzer S, Levander C, Elvin A, Lärfars G, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma. 2007; 21:52–7.
Article2. Patel A, Ogawa B, Charlton T, Thordarson D. Incidence of deep vein thrombosis and pulmonary embolism after Achilles tendon rupture. Clin Orthop Relat Res. 2012; 470:270–4.
Article3. Coon WW. Venous thromboembolism. Prevalence, risk factors, and prevention. Clin Chest Med. 1984; 5:391–401.41. Makhdom AM, Cota A, Saran N, Chaytor R. Incidence of symptomatic deep venous thrombosis after Achilles tendon rupture. J Foot Ankle Surg. 2013; 52:584–7.
Article5. Nilsson-Helander K, Thurin A, Karlsson J, Eriksson BI. High incidence of deep venous thrombosis after Achilles tendon rupture: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2009; 17:1234–8.
Article6. Felcher AH, Mularski RA, Mosen DM, Kimes TM, DeLoughery TG, Laxson SE. Incidence and risk factors for venous thromboembolic disease in podiatric surgery. Chest. 2009; 135:917–22.
Article7. Howell MD, Geraci JM, Knowlton AA. Congestive heart failure and outpatient risk of venous thromboembolism: a retrospective, case-control study. J Clin Epidemiol. 2001; 54:810–6.
Article8. Di Nisio M, Di Iorio A, Porreca E, Abate M, Ferrante N, Bandinelli S, et al. Obesity, poor muscle strength, and venous thromboembolism in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2011; 66:320–5.
Article9. Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. American College of Chest Physicians. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e278S–325S.10. Lassen MR, Borris LC, Nakov RL. Use of the low-molecular-weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med. 2002; 347:726–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Massive Defect in Achilles Tendon with Tendon Allograft: A Case Report
- Heterotopic Ossification of a Partially Ruptured Achilles Tendon (A Case Report)
- A Comparative Study of Surgical Treatment in the Ruptured Achilles Tendon: Minimal incision and Open repair
- Long Term Result of Four Cases without a Staged Reconstruction of an Infected Achilles Tendon Following Repair
- A Comparative Study of Surgical Treatment Result in the Ruptured Achilles Tendon: Minimal Incision Percutaneous Repair and Open Repair