Yonsei Med J.
2013 Jul;54(4):912-920. 10.3349/ymj.2013.54.4.912.
Pure Laparoscopic Radical Cystectomy with Ileal Conduit: A Single Surgeon's Mid-Term Outcomes
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. siseo@skku.edu
- 2Institute for Refractory Cancer Research, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Urology, Kangnam General Hospital, Yongin, Korea.
- KMID: 2158226
- DOI: http://doi.org/10.3349/ymj.2013.54.4.912
Abstract
- PURPOSE
The use of laparoscopic radical cystectomy (LRC) for muscle-invasive bladder cancer is not yet widespread because of the technical difficulties of the procedure and the lengthy operating time. In this study, we report a single surgeon's experience with LRC.
MATERIALS AND METHODS
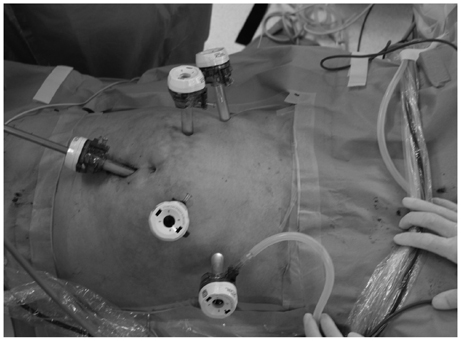
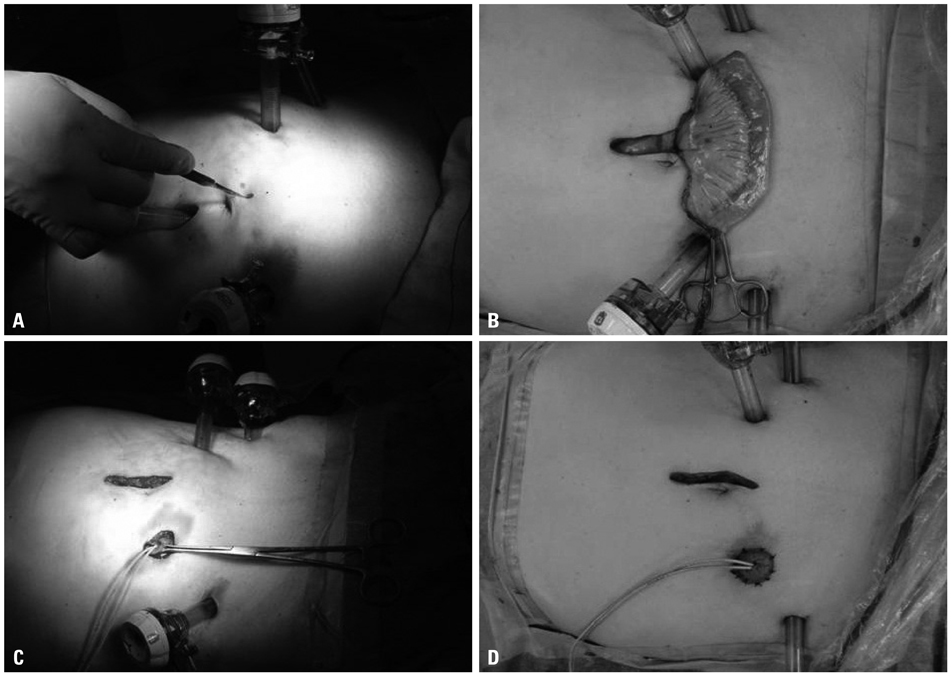
Thirty patients (25 men and 5 women) with bladder cancer underwent LRC and ileal conduit by a single surgeon between November 2007 and May 2011. An extracorporeal urinary diversion was performed through 5-6 cm midline incision for specimen extraction.
RESULTS
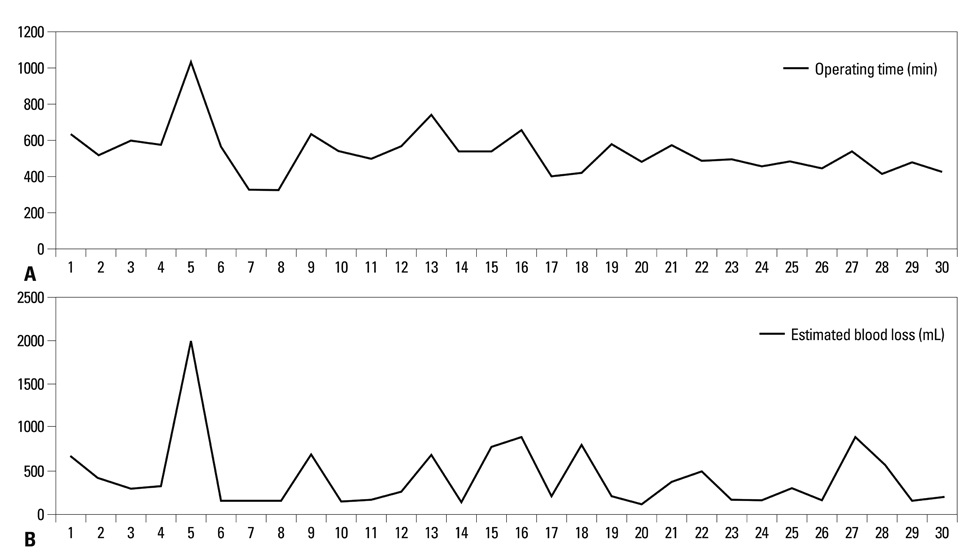
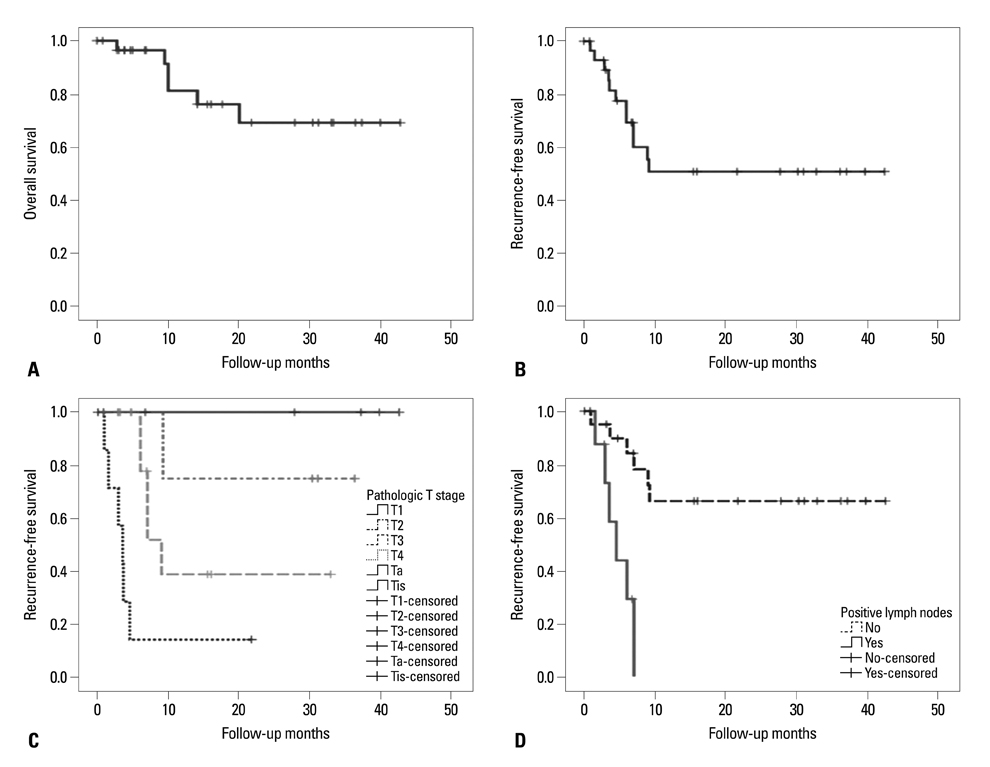
The median operating time and estimated blood loss were 527.5 minutes and 275 mL, respectively. There was no conversion to open surgery. The median time to oral intake and postoperative hospital stay were 5 days and 12 days, respectively. The rates of immediate, early postoperative and late postoperative complication were 3.3%, 20% and 20%, respectively. With 16 months of median follow-up, the overall and recurrence-free survival rates were 70% and 56.7%, respectively.
CONCLUSION
LRC is feasible for the management of invasive bladder cancer and, with appropriate patient selection, can be a good alternative to open or robot-assisted radical cystectomy in the era of robot-assisted surgery.
MeSH Terms
Figure
Reference
-
1. Khan MS, Elhage O, Challacombe B, Rimington P, Murphy D, Dasgupta P. Analysis of early complications of robotic-assisted radical cystectomy using a standardized reporting system. Urology. 2011; 77:357–362.
Article2. Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001; 19:666–675.
Article3. Studer UE, Burkhard FC, Schumacher M, Kessler TM, Thoeny H, Fleischmann A, et al. Twenty years experience with an ileal orthotopic low pressure bladder substitute--lessons to be learned. J Urol. 2006; 176:161–166.
Article4. Cathelineau X, Arroyo C, Rozet F, Barret E, Vallancien G. Laparoscopic assisted radical cystectomy: the montsouris experience after 84 cases. Eur Urol. 2005; 47:780–784.
Article5. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.6. Gill IS, Fergany A, Klein EA, Kaouk JH, Sung GT, Meraney AM, et al. Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology. 2000; 56:26–29.
Article7. Hemal AK, Singh I, Kumar R. Laparoscopic radical cystectomy and ileal conduit reconstruction: preliminary experience. J Endourol. 2003; 17:911–916.
Article8. Simonato A, Gregori A, Lissiani A, Bozzola A, Galli S, Gaboardi F. Laparoscopic radical cystoprostatectomy: our experience in a consecutive series of 10 patients with a 3 years follow-up. Eur Urol. 2005; 47:785–790.
Article9. Moinzadeh A, Gill IS, Desai M, Finelli A, Falcone T, Kaouk J. Laparoscopic radical cystectomy in the female. J Urol. 2005; 173:1912–1917.
Article10. Castillo OA, Abreu SC, Mariano MB, Tefilli MV, Hoyos J, Pinto I, et al. Complications in laparoscopic radical cystectomy. The South American experience with 59 cases. Int Braz J Urol. 2006; 32:300–305.
Article11. Gerullis H, Kuemmel C, Popken G. Laparoscopic cystectomy with extracorporeal-assisted urinary diversion: experience with 34 patients. Eur Urol. 2007; 51:193–198.
Article12. Gao ZL, Fan J, Zhao JJ, Xia SJ, Shi L, Men CP, et al. Laparoscopic radical cystectomy with extracorporeal ileal conduit urinary diversion for treatment of Chinese bladder cancer patients. Urol Int. 2007; 79:204–209.
Article13. Hemal AK, Kolla SB. Comparison of laparoscopic and open radical cystoprostatectomy for localized bladder cancer with 3-year oncological followup: a single surgeon experience. J Urol. 2007; 178:2340–2343.
Article14. Makiyama K, Nakaigawa N, Murakami T, Hayashi N, Sano F, Kawahara T, et al. [Perioperative outcome of laparoscopic radical cystectomy: comparison to open radical cystectomy]. Nihon Hinyokika Gakkai Zasshi. 2010; 101:721–725.
Article15. Ha US, Kim SI, Kim SJ, Cho HJ, Hong SH, Lee JY, et al. Laparoscopic versus open radical cystectomy for the management of bladder cancer: mid-term oncological outcome. Int J Urol. 2010; 17:55–61.
Article16. Huang J, Lin T, Liu H, Xu K, Zhang C, Jiang C, et al. Laparoscopic radical cystectomy with orthotopic ileal neobladder for bladder cancer: oncologic results of 171 cases with a median 3-year follow-up. Eur Urol. 2010; 58:442–449.
Article17. Guru KA, Hussain A, Chandrasekhar R, Piacente P, Hussain A, Chandrasekhar R, et al. Current status of robot-assisted surgery in urology: a multi-national survey of 297 urologic surgeons. Can J Urol. 2009; 16:4736–4741.18. Abraham JB, Young JL, Box GN, Lee HJ, Deane LA, Ornstein DK. Comparative analysis of laparoscopic and robot-assisted radical cystectomy with ileal conduit urinary diversion. J Endourol. 2007; 21:1473–1480.
Article19. Smith A, Kurpad R, Lal A, Nielsen M, Wallen EM, Pruthi RS. Cost analysis of robotic versus open radical cystectomy for bladder cancer. J Urol. 2010; 183:505–509.
Article20. Gregori A, Galli S, Goumas I, Scieri F, Stener S, Gaboardi F. A cost comparison of laparoscopic versus open radical cystoprostatectomy and orthotopic ileal neobladder at a single institution. Arch Ital Urol Androl. 2007; 79:127–129.21. Novotny V, Hakenberg OW, Wiessner D, Heberling U, Litz RJ, Oehlschlaeger S, et al. Perioperative complications of radical cystectomy in a contemporary series. Eur Urol. 2007; 51:397–401.
Article22. Shabsigh A, Korets R, Vora KC, Brooks CM, Cronin AM, Savage C, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol. 2009; 55:164–174.
Article23. Hautmann RE, de Petriconi RC, Volkmer BG. Lessons learned from 1,000 neobladders: the 90-day complication rate. J Urol. 2010; 184:990–994.
Article24. Sung HH, Ahn JS, Seo SI, Jeon SS, Choi HY, Lee HM, et al. A comparison of early complications between open and robot-assisted radical cystectomy. J Endourol. 2012; 26:670–675.
Article25. Orvieto MA, DeCastro GJ, Trinh QD, Jeldres C, Katz MH, Patel VR, et al. Oncological and functional outcomes after robot-assisted radical cystectomy: critical review of current status. Urology. 2011; 78:977–984.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fistula between Ileal Conduit and Iliac Artery after Radical Cystectomy with Ileal Conduit Urinary Diversion
- Body Image Following Radical Cystectomy and Ileal Neobladder or Conduit in Korean Patients
- Short Term Outcomes of Laparoscopic Radical Cystectomy with an Extracorporeal Ileal Conduit: Comparative Analysis with the Open Method
- A Study on Complications of Cystectomies and Urinary Diversions
- Safety of Adjuvant Chemotherapy after Orthotopic Bladder Substitution: Comparison to Ileal Conduit