Yonsei Med J.
2008 Oct;49(5):860-863. 10.3349/ymj.2008.49.5.860.
Extranodal Marginal Zone Lymphoma Occurring along the Trachea and Central Airway
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea. youngkim@catholic.ac.kr
- 2Department of Radiology, The Catholic University of Korea, Seoul, Korea.
- 3Department of Clinical Pathology, The Catholic University of Korea, Seoul, Korea.
- KMID: 2158208
- DOI: http://doi.org/10.3349/ymj.2008.49.5.860
Abstract
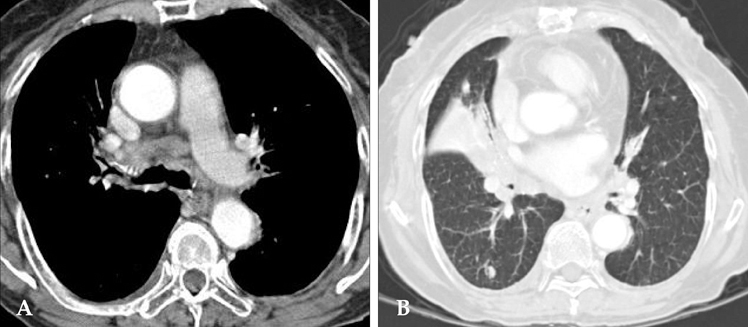
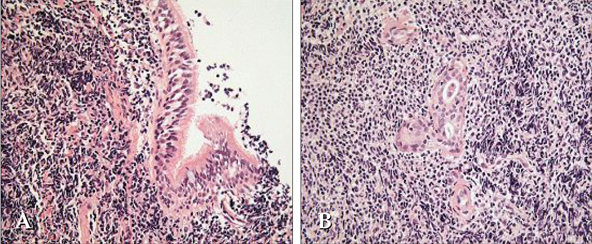
- Extranodal marginal zone lymphoma is a low-grade B cell lymphoma that presents with an indolent clinicopathologic nature. Although this tumor can occur in various sites, including the gastrointestinal tract and lungs, it develops and spreads extremely rarely along the trachea and central airway. We report a case of extranodal lymphoma of mucosa-associated lymphoid tissue with tracheobronchial involvement. An 83-year-old woman presented with a cough and dyspnea. Bronchoscopic evaluation confirmed diffuse, multiple nodular lesions in both the trachea and large bronchi, and she was diagnosed with an extranodal marginal zone lymphoma of the tracheobronchial tree. After systemic chemotherapy, she survived for more than 18 months.
Keyword
MeSH Terms
Figure
Reference
-
1. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983. 52:1410–1416.
Article2. Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000. 95:802–806.
Article3. Zinzani PL, Magagnoli M, Galieni P, Martelli M, Poletti V, Zaja F, et al. Nongastrointestinal low-grade mucosa-associated lymphoid tissue lymphoma: analysis of 75 patients. J Clin Oncol. 1999. 17:1254.4. Fidias P, Wright C, Harris NL, Urba W, Grossbard ML. Primary tracheal non-Hodgkin's lymphoma. A case report and review of the literature. Cancer. 1996. 77:2332–2338.
Article5. Ahmed S, Kussick SJ, Siddiqui AK, Bhuiya TA, Khan A, Sarewitz S, et al. Bronchial-associated lymphoid tissue lymphoma: a clinical study of a rare disease. Eur J Cancer. 2004. 40:1320–1326.
Article6. Cordier JF, Chailleux E, Lauque D, Reynaud-Gaubert M, Dietemann-Molard A, Dalphin JC, et al. Primary pulmonary lymphomas. A clinical study of 70 cases in nonimmunocompromised patients. Chest. 1993. 103:201–208.7. Lee DK, Im JG, Lee KS, Lee JS, Seo JB, Goo JM, et al. B-cell lymphoma of bronchus-associated lymphoid tissue (BALT): CT features in 10 patients. J Comput Assist Tomogr. 2000. 24:30–34.
Article8. Sankaranarayanan V, Zeidalski TM, Chitkara RK. A 55-year-old smoker with a persistent right lower lobe infiltrate. Chest. 2005. 127:2266–2270.
Article9. Bae YA, Lee KS, Han J, Ko YH, Kim BT, Chung MJ, et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: imaging findings in 21 patients. Chest. 2008. 133:433–440.
Article10. Solomonov A, Zuckerman T, Goralnik L, Ben-Arieh Y, Rowe JM, Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol. 2008. 83:416–419.
Article11. Bienenstock J, Johnston N, Perey DY. Bronchial lymphoid tissue. I. Morphologic characteristics. Lab Invest. 1973. 28:686–692.12. Pabst R. Is BALT a major component of the human lung immune system? Immunol Today. 1992. 13:119–122.
Article13. Sminia T, van der Brugge-Gamelkoorn GJ, Jeurissen SH. Structure and function of bronchus-associated lymphoid tissue (BALT). Crit Rev Immunol. 1989. 9:119–150.14. Okubo K, Miyamoto N, Komaki C. Primary mucosa-associated lymphoid tissue (MALT) lymphoma of the trachea: a case of surgical resection and long term survival. Thorax. 2005. 60:82–83.
Article15. Kaplan MA, Pettit CL, Zukerberg LR, Harris NL. Primary lymphoma of the trachea with morphologic and immunophenotypic characteristics of low-grade B-cell lymphoma of mucosa-associated lymphoid tissue. Am J Surg Pathol. 1992. 16:71–75.
Article16. Wiggins J, Sheffield E, Green M. Primary B cell malignant lymphoma of the trachea. Thorax. 1988. 43:497–498.
Article17. Tsurutani J, Kinoshita A, Kaida H, Fujii H, Narasaki F, Fukuda M, et al. Bronchoscopic therapy for mucosa-associated lymphoid tissue lymphoma of the trachea. Intern Med. 1999. 38:276–278.
Article18. Gómez-Román JJ, Pérez-Montes R, Pérez-Expósito MA, Richard C, Baro J, Val-Bernal JF. Primary lymphoplasmacytoid lymphoma of the trachea with immunoglobulin G paraprotein. Pathol Int. 1999. 49:1100–1104.
Article19. Johnson V, Burrows NJ, Ali NJ, Cox G. B cell non-Hodgkin's lymphoma of the trachea mimicking COPD. Thorax. 2004. 59:1100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- A Case of Primary Malignant Lymphoma of Trachea
- Clinical Study of Ocular Adnexal Extranodal Marginal Zone B-cell Lymphoma: From the Perspective of Dermatology
- A Case of Synchronous Lung Adenocarcinoma and Extranodal Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type
- A case of nodal marginal zone B-cell lymphoma of the lower eyelid