Yonsei Med J.
2007 Aug;48(4):704-710. 10.3349/ymj.2007.48.4.704.
Congenital Cavernous Sinus Cystic Teratoma
- Affiliations
-
- 1Department of Neurosurgery, Brain Korea 21 Project for Medical Science, Brain Research Institute, Yonsei University College of Medicine, Seoul, Korea. dskim33@yuhs.ac
- 2Departments of Pathology, Brain Korea 21 Project for Medical Science, Brain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2158179
- DOI: http://doi.org/10.3349/ymj.2007.48.4.704
Abstract
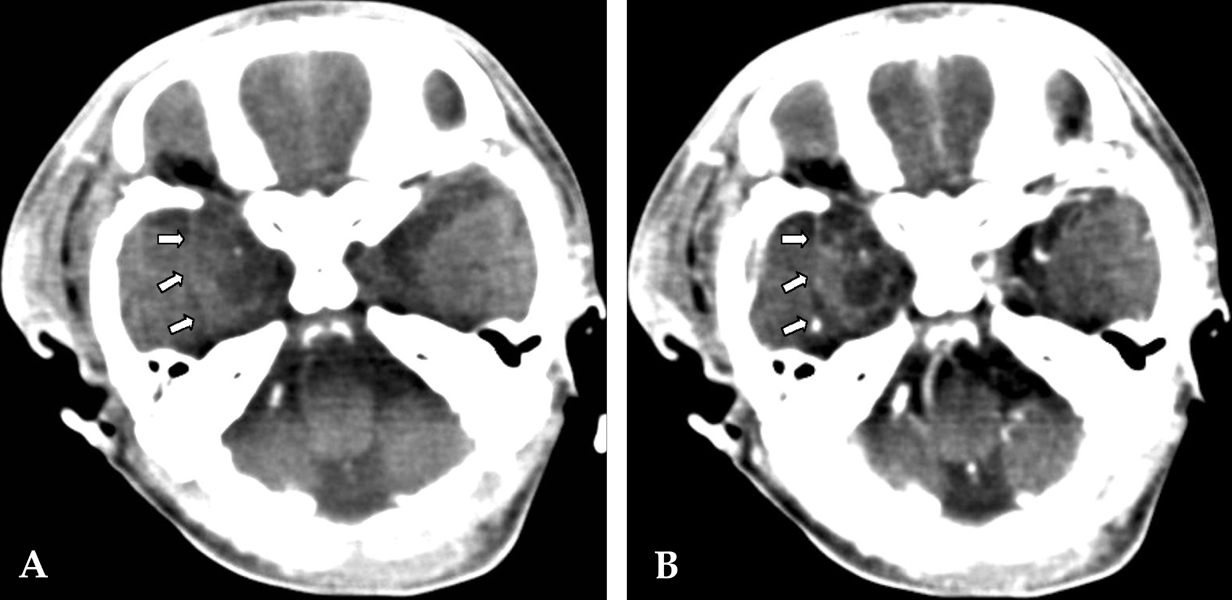
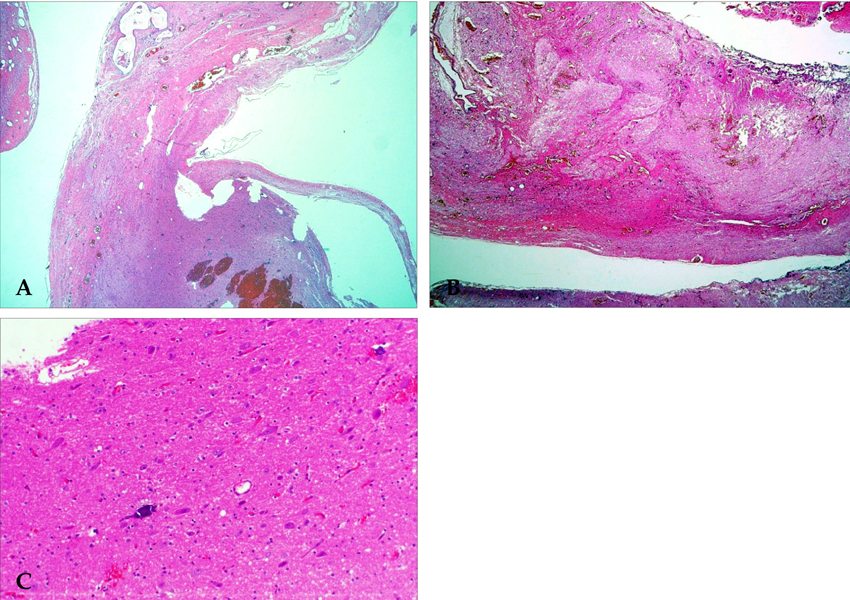
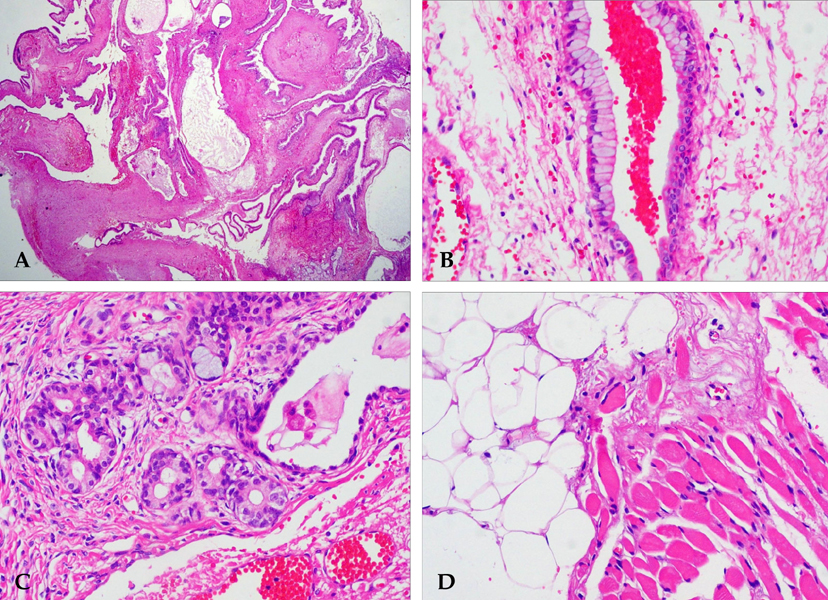
- Teratomas represent 0.5% of all intracranial tumors. These benign tumors contain tissue representative of the three germinal layers. Most teratomas are midline tumors located predominantly in the sellar and pineal regions. The presence of a teratoma in the cavernous sinus is very rare. Congenital teratomas are also rare, especially those of a cystic nature. To our knowledge, this would be the first case report of a congenital, rapidly growing cystic teratoma within the cavernous sinus. A three-month-old boy presented with a past medical history of easy irritability and poor oral intake. A magnetic resonance image (MRI) scan of the head disclosed a large expanding cystic tumor filling the right cavernous sinus and extending into the pterygopalatine fossa through the foramen rotundum. These scans also demonstrated a small area of mixed signal intensity, the result of the different tissue types conforming to the tumor. Heterogeneous enhancement was seen after the infusion of contrast medium. However, this was a cystic tumor with a large cystic portion. Thus, a presumptive diagnosis of cystic glioma was made. With the use of a right frontotemporal approach, extradural dissection of the tumor was performed. The lesion entirely occupied the cavernous sinus, medially displacing the Gasserian ganglion and trigeminal branches (predominantly V1 and V2). The lesion was composed of different tissues, including fat, muscle and mature, brain-like tissue. The tumor was completely removed, and the pathological report confirmed the diagnosis of a mature teratoma. There was no evidence of recurrence. Despite the location of the lesion in the cavernous sinus, total removal can be achieved with the use of standard microsurgical techniques.
Keyword
MeSH Terms
Figure
Reference
-
1. Becherer TA, Davis DG, Hodes JE, Warf BC. Intracavernous teratoma in a school-aged child. Pediatr Neurosurg. 1999. 30:135–139.
Article2. Pikus HJ, Holmes B, Harbaugh RE. Teratoma of the cavernous sinus: case report. Neurosurgery. 1995. 36:1020–1023.3. Tobias S, Valarezo J, Meir K, Umansky F. Giant cavernous sinus teratoma: a clinical example of a rare entity: case report. Neurosurgery. 2001. 48:1367–1371.
Article4. Shaffrey ME, Lanzino G, Lopes MB, Hessler RB, Kassell NF, VandenBerg SR. Maturation of intracranial immature teratomas. Report of two cases. J Neurosurg. 1996. 85:672–676.5. Hunt SJ, Johnson PC, Coons SW, Pittman HW. Neonatal intracranial teratomas. Surg Neurol. 1990. 34:336–342.
Article6. Wakai S, Arai T, Nagai M. Congenital brain tumors. Surg Neurol. 1984. 21:597–609.
Article7. Di Rocco C, Iannelli A, Ceddia A. Intracranial tumors of the first year of life. A cooperative survey of the 1986-1987 Education Committee of the ISPN. Childs Nerv Syst. 1991. 7:150–153.8. Nanda A, Schut L, Sutton LN. Congenital forms of intracranial teratoma. Childs Nerv Syst. 1991. 7:112–114.
Article9. Sano K. Pathogenesis of intracranial germ cell tumors reconsidered. J Neurosurg. 1999. 90:258–264.
Article10. Keene DL, Hsu E, Ventureyra E. Brain tumors in childhood and adolescence. Pediatr Neurol. 1999. 20:198–203.
Article11. Lesoin F, Jomin M. Direct microsurgical approach to intracavernous tumors. Surg Neurol. 1987. 28:17–22.
Article12. Canan A, Glsevin T, Nejat A, Tezer K, Sule Y, Meryem T, et al. Neonatal intracranial teratoma. Brain Dev. 2000. 22:340–342.
Article13. Lipman SP, Pretorius DH, Rumack CM, Manco-Johnson ML. Fetal intracranial teratoma: US diagnosis of three cases and a review of the literature. Radiology. 1985. 157:491–494.
Article14. Matsutani M, Sano K, Takakura K, Fujimaki T, Nakamura O, Funata N, et al. Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg. 1997. 86:446–455.
Article15. Jennings MT, Gelman R, Hochberg F. Intracranial germ-cell tumors: natural history and pathogenesis. J Neurosurg. 1985. 63:155–167.
Article16. Im SH, Wang KC, Kim SK, Lee YH, Chi JG, Cho BK. Congenital intracranial teratoma: prenatal diagnosis and postnatal successful resection. Med Pediatr Oncol. 2003. 40:57–61.
Article17. Kang MK, Ahn YC, Park JO, Han J, Lee KS. Lung metastasis from an immature teratoma of the nasal cavity masquerading a small cell carcinoma of the lung. Yonsei Med J. 2006. 47:571–574.
Article18. Shim KW, Kim DS, Choi JU. Mixed or metachronous germ cell tumor? Childs Nerv Syst. 2007. 23:713–718.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Presacral Cystic Teratoma
- A Case of Cystic Teratoma on the Floor of the Mouth in Neonate
- Endodermal Sinus Tumor Arising from Resected Benign Cystic Sacrococcygeal Teratoma
- A Case of Cavernous Sinus Thrombophlebitis Secondary toAcute Isolated Sphenoid Sinusitis
- Congenital Hydrocolpos Mimicking a Mature Cystic Teratoma in the Pelvis