J Korean Med Sci.
2012 Nov;27(11):1391-1397. 10.3346/jkms.2012.27.11.1391.
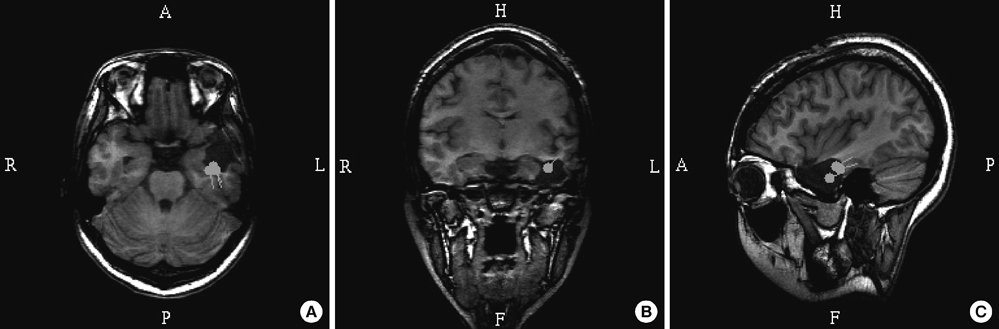
Localization Value of Magnetoencephalography Interictal Spikes in Adult Nonlesional Neocortical Epilepsy
- Affiliations
-
- 1MEG Center, Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea. chungc@snu.ac.kr
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 3Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 4Research Center for Sensory Organs, Seoul National University, Seoul, Korea.
- KMID: 2157952
- DOI: http://doi.org/10.3346/jkms.2012.27.11.1391
Abstract
- Few studies have included magnetoencephalography (MEG) when assessing the diagnostic value of presurgical modalities in a nonlesional epilepsy population. Here, we compare single photon emission computed tomography (SPECT), positron emission tomography (PET), video-EEG (VEEG), and MEG, with intracranial EEG (iEEG) to determine the value of individual modalities to surgical decisions. We analyzed 23 adult epilepsy patients with no abnormal MRI findings who had undergone surgical resection. Localization of individual presurgical tests was determined for hemispheric and lobar locations based on visual analysis. Each localization result was compared with the ictal onset zone (IOZ) defined by using iEEG. The highest to the lowest hemispheric concordance rates were MEG (83%) > ictal VEEG (78%) > PET (70%) > ictal SPECT (57%). The highest to lowest lobar concordance rates were ictal VEEG = MEG (65%) > PET (57%) > ictal SPECT (52%). Statistical analysis showed MEG to have a higher hemispheric concordance than that of ictal SPECT (P = 0.031). We analyzed the effects of MEG clustered-area resection on surgical outcome. Patients who had resection of MEG clusters showed a better surgical outcome than those without such resection (P = 0.038). It is suggested that MEG-based localization had the highest concordance with the iEEG-defined IOZ. Furthermore, MEG cluster resection has prognostic significance in predicting surgical outcome.
MeSH Terms
Figure
Reference
-
1. Berkovic SF, McIntosh AM, Kalnins RM, Jackson GD, Fabinyi GC, Brazenor GA, Bladin PF, Hopper JL. Preoperative MRI predicts outcome of temporal lobectomy: an actuarial analysis. Neurology. 1995. 45:1358–1363.2. Tonini C, Beghi E, Berg AT, Bogliun G, Giordano L, Newton RW, Tetto A, Vitelli E, Vitezic D, Wiebe S. Predictors of epilepsy surgery outcome: a meta-analysis. Epilepsy Res. 2004. 62:75–87.3. Yun CH, Lee SK, Lee SY, Kim KK, Jeong SW, Chung CK. Prognostic factors in neocortical epilepsy surgery: multivariate analysis. Epilepsia. 2006. 47:574–579.4. Semah F, Picot MC, Adam C, Broglin D, Arzimanoglou A, Bazin B, Cavalcanti D, Baulac M. Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology. 1998. 51:1256–1262.5. Duncan JS. Imaging and epilepsy. Brain. 1997. 120:339–377.6. Lee SK, Lee SY, Kim KK, Hong KS, Lee DS, Chung CK. Surgical outcome and prognostic factors of cryptogenic neocortical epilepsy. Ann Neurol. 2005. 58:525–532.7. Holmes MD, Born DE, Kutsy RL, Wilensky AJ, Ojemann GA, Ojemann LM. Outcome after surgery in patients with refractory temporal lobe epilepsy and normal MRI. Seizure. 2000. 9:407–411.8. Alarcon G, Valentin A, Watt C, Selway RP, Lacruz ME, Elwes RD, Jarosz JM, Honavar M, Brunhuber F, Mullatti N, et al. Is it worth pursuing surgery for epilepsy in patients with normal neuroimaging? J Neurol Neurosurg Psychiatry. 2006. 77:474–480.9. Vinton AB, Carne R, Hicks RJ, Desmond PM, Kilpatrick C, Kaye AH, O'Brien TJ. The extent of resection of FDG-PET hypometabolism relates to outcome of temporal lobectomy. Brain. 2007. 130:548–560.10. Chassoux F, Rodrigo S, Semah F, Beuvon F, Landre E, Devaux B, Turak B, Mellerio C, Meder JF, Roux FX, et al. FDG-PET improves surgical outcome in negative MRI Taylor-type focal cortical dysplasias. Neurology. 2010. 75:2168–2175.11. von Oertzen TJ, Mormann F, Urbach H, Reichmann K, Koenig R, Clusmann H, Biersack HJ, Elger CE. Prospective use of subtraction ictal SPECT coregistered to MRI (SISCOM) in presurgical evaluation of epilepsy. Epilepsia. 2011. 52:2239–2248.12. Seo JH, Holland K, Rose D, Rozhkov L, Fujiwara H, Byars A, Arthur T, DeGrauw T, Leach JL, Gelfand MJ, et al. Multimodality imaging in the surgical treatment of children with nonlesional epilepsy. Neurology. 2011. 76:41–48.13. Garcia-Morales I, Maestu F, Perez-Jimenez MA, Elices E, Ortiz T, Alvarez-Linera J, Gil-Nagel A. A clinical and magnetoencephalography study of MRI-negative startle epilepsy. Epilepsy Behav. 2009. 16:166–171.14. Ramachandrannair R, Otsubo H, Shroff MM, Ochi A, Weiss SK, Rutka JT, Snead OC 3rd. MEG predicts outcome following surgery for intractable epilepsy in children with normal or nonfocal MRI findings. Epilepsia. 2007. 48:149–157.15. Funke ME, Moore K, Orrison WW Jr, Lewine JD. The role of magnetoencephalography in "nonlesional" epilepsy. Epilepsia. 2011. 52:10–14.16. Zhang R, Wu T, Wang Y, Liu H, Zou Y, Liu W, Xiang J, Xiao C, Yang L, Fu Z. Interictal magnetoencephalographic findings related with surgical outcomes in lesional and nonlesional neocortical epilepsy. Seizure. 2011. 20:692–700.17. Jeong W, Chung CK, Kim JS. MEG interictal spike clustering in relation with surgical outcome of cortical dysplasia. J Korean Neurosurg Soc. in press.18. Brodbeck V, Spinelli L, Lascano AM, Pollo C, Schaller K, Vargas MI, Wissmeyer M, Michel CM, Seeck M. Electrical source imaging for presurgical focus localization in epilepsy patients with normal MRI. Epilepsia. 2010. 51:583–591.19. Wheless JW, Willmore LJ, Breier JI, Kataki M, Smith JR, King DW, Meador KJ, Park YD, Loring DW, Clifton GL, et al. A comparison of magnetoencephalography, MRI, and V-EEG in patients evaluated for epilepsy surgery. Epilepsia. 1999. 40:931–941.20. Stefan H, Hummel C, Hopfengartner R, Pauli E, Tilz C, Ganslandt O, Kober H, Moler A, Buchfelder M. Magnetoencephalography in extratemporal epilepsy. J Clin Neurophysiol. 2000. 17:190–200.21. Moore KR, Funke ME, Constantino T, Katzman GL, Lewine JD. Magnetoencephalographically directed review of high-spatial-resolution surface-coil MR images improves lesion detection in patients with extratemporal epilepsy. Radiology. 2002. 225:880–887.22. Moeller F, Tyvaert L, Nguyen DK, LeVan P, Bouthillier A, Kobayashi E, Tampieri D, Dubeau F, Gotman J. EEG-fMRI: adding to standard evaluations of patients with nonlesional frontal lobe epilepsy. Neurology. 2009. 73:2023–2030.23. Lee JJ, Lee SK, Lee SY, Park KI, Kim DW, Lee DS, Chung CK, Nam HW. Frontal lobe epilepsy: clinical characteristics, surgical outcomes and diagnostic modalities. Seizure. 2008. 17:514–523.24. Kellinghaus C, Luders HO. Frontal lobe epilepsy. Epileptic Disord. 2004. 6:223–239.25. Jeha LE, Najm I, Bingaman W, Dinner D, Widdess-Walsh P, Luders H. Surgical outcome and prognostic factors of frontal lobe epilepsy surgery. Brain. 2007. 130:574–584.26. Chung CK, Lee SK, Kim KJ. Surgical outcome of epilepsy caused by cortical dysplasia. Epilepsia. 2005. 46:Suppl 1. 25–29.27. Krsek P, Maton B, Korman B, Pacheco-Jacome E, Jayakar P, Dunoyer C, Rey G, Morrison G, Ragheb J, Vinters HV, et al. Different features of histopathological subtypes of pediatric focal cortical dysplasia. Ann Neurol. 2008. 63:758–769.28. Nobili L, Francione S, Mai R, Cardinale F, Castana L, Tassi L, Sartori I, Didato G, Citterio A, Colombo N, et al. Surgical treatment of drug-resistant nocturnal frontal lobe epilepsy. Brain. 2007. 130:561–573.29. Hong KS, Lee SK, Kim JY, Lee DS, Chung CK. Pre-surgical evaluation and surgical outcome of 41 patients with non-lesional neocortical epilepsy. Seizure. 2002. 11:184–192.30. McGonigal A, Bartolomei F, Regis J, Guye M, Gavaret M, Trebuchon-Da Fonseca A, Dufour H, Figarella-Branger D, Girard N, Peragut JC, et al. Stereoelectroencephalography in presurgical assessment of MRI-negative epilepsy. Brain. 2007. 130:3169–3183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of Magnetoencephalography in Children
- Magnetoencephalography in Epilepsy
- Magnetoencephalography Interictal Spike Clustering in Relation with Surgical Outcome of Cortical Dysplasia
- Magnetoencephalography in pediatric epilepsy
- Dipole Source Localization and Low Resolution Electromagnetic Tomography(LORETA) of Interictal Spikes in Mesial and Lateral Temporal Lobe Epilepsy