J Korean Med Sci.
2005 Dec;20(6):1085-1088. 10.3346/jkms.2005.20.6.1085.
A Catastrophic-Onset Longitudinal Myelitis Accompanied by Bilateral Internuclear Ophthalmoplegia in a Patient with Systemic Lupus Erythematosus
- Affiliations
-
- 1Department of Internal Medicine, Chonbuk National University Medical School, and Research Institute of Clinical Medicine, Jeonju, Korea. goldgu@chonbuk.ac.kr
- KMID: 2157770
- DOI: http://doi.org/10.3346/jkms.2005.20.6.1085
Abstract
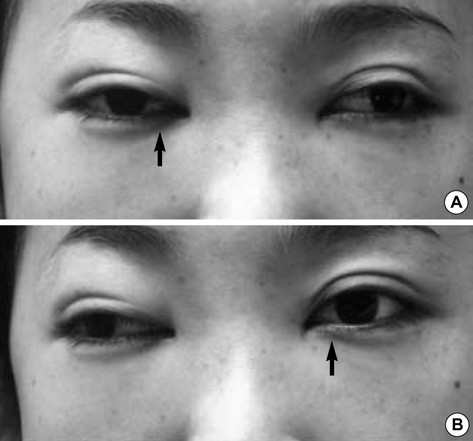
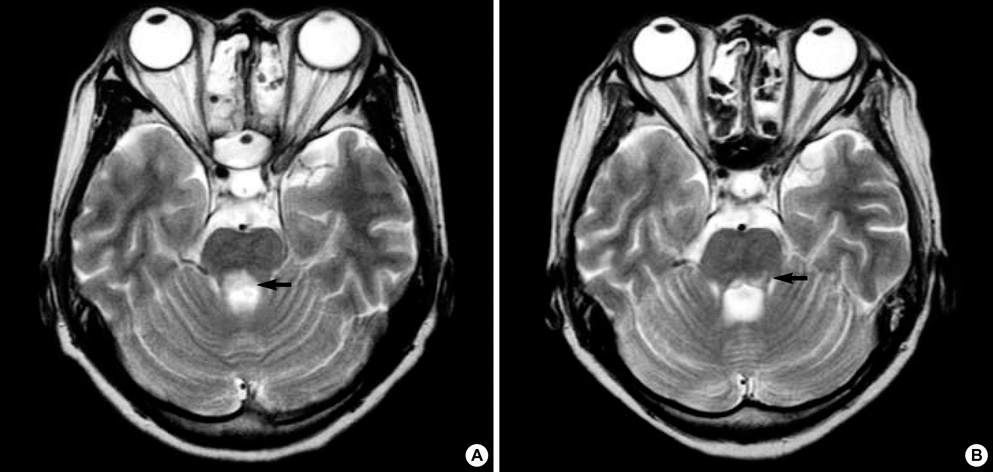
- Transverse myelitis (TM) extending from midbrain to the entire spinal cord accompanied by internuclear ophthalmoplegia is extremely rare but cause serious central nervous system complications in patients with systemic lupus erythematosus. We report a case of a 28-yr-old woman with TM extending from the midbrain to the conus medullaris longitudinally and internuclear ophthalmoplegia associated with systemic lupus erythematosus. Her neurological symptoms had an abrupt catastrophic onset and rapidly progressed to respiratory failure within 24 hr. Bilateral internuclear ophthalmoplegia was also followed by TM. Brain MR images showed definite brainstem lesions, which were deeply associated with internuclear ophthalmoplegia, and diffuse signal changes in the whole spinal cord, medulla, pons and midbrain. Clinical improvement of her ophthalmoplegia and of neurological dysfunction of the upper extremities was noted after prompt and aggressive treatment with intravenous pulsed methylprednisolone and cyclophosphamide. However, the neurological dysfunction of the lower limbs and bladder and colon paralysis were almost unchanged until six months passed.
Keyword
MeSH Terms
Figure
Reference
-
1. Cho BK, Song JS, Bae SK, Yoon SJ, Park W. A case of transverse myelitis as a first manifestation of systemic lupus erythematosus. J Korean Rheum Assoc. 2000. 7:263–267.2. Andrianakos AA, Duffy J, Suzuki M, Sharp JT. Transverse myelopathy in systemic lupus erythematosus: report of three cases and review of the literature. Ann Intern Med. 1975. 83:616–624.3. Ropper AH, Poskanzer DC. The prognosis of acute and subacute transverse myelopathy based on early signs and symptoms. Ann Neurol. 1978. 4:51–59.
Article4. Ko HY, Kwon DR, Jo SC, Yang JH. Extensive longitudinal myelitis associated with systemic lupus erythematosus: a case report. J Korean Acad Rehabil Med. 2003. 27:1004–1006.5. Tellez-Zenteno JF, Remes-Troche JM, Negrete-Pulido RO, Davila-Maldonado L. Longitudinal myelitis associated with systemic lupus erythematosus: clinical features and magnetic resonance imaging of six cases. Lupus. 2001. 10:851–856.6. Neumann-Andersen G, Lindgren S. Involvement of the entire spinal cord and medulla oblongata in acute catastrophic-onset transverse myelitis in SLE. Clin Rheumatol. 2000. 19:156–160.
Article7. Inslicht DV, Stein AB, Pomerantz F, Ragnarsson KT. Three women with lupus transverse myelitis: case reports and differential diagnosis. Arch Phys Med Rehabil. 1998. 79:456–459.
Article8. Zee DS. Internuclear ophthalmoplegia: pathophysiology and diagnosis. Baillieres Clin Neurol. 1992. 1:455–470.9. Galindo M, Pablos JL, Gomez-Reino JJ. Internuclear ophthalmoplegia in systemic lupus erythematosus. Semin Arthritis Rheum. 1998. 28:179–186.
Article10. West SG. Neuropsychiatric lupus. Rheum Dis Clin North Am. 1994. 20:129–158.11. Deodhar AA, Hochenedel T, Bennett RM. Longitudinal involvement of the spinal cord in a patient with lupus related transverse myelitis. J Rheumatol. 1999. 26:446–449.12. Lessell S. The neuro-ophthalmology of systemic lupus erythematosus. Doc Ophthalmol. 1979. 47:13–42.
Article13. Cogen MS, Kline LB, Duvall ER. Bilateral internuclear ophthalmoplegia in systemic lupus erythematosus. J Clin Neuroophthalmol. 1987. 7:69–73.14. McCune WJ, Golbus J. Neuropsychiatric lupus. Rheum Dis Clin North Am. 1988. 14:149–167.15. Lavalle C, Pizarro S, Drenkard C, Sanchez-Guerrero J, Alarcon-Segovia D. Transverse myelitis: a manifestation of systemic lupus erythematosus strongly associated with antiphospholipid antibodies. J Rheumatol. 1990. 17:34–37.16. Kovacs B, Lafferty TL, Brent LH, DeHoratius RJ. Transverse myelopathy in systemic lupus erythematosus: an analysis of 14 cases and review of the literature. Ann Rheum Dis. 2000. 59:120–124.
Article17. Harisdangkul V, Doorenbos D, Subramony SH. Lupus transverse myelopathy: better outcome with early recognition and aggressive high-dose intravenous corticosteroid pulse treatment. J Neurol. 1995. 242:326–331.
Article18. Barile L, Lavalle C. Transverse myelitis in systemic lupus erythematosus: the effect of IV pulse methylprednisolone and cyclophosphamide. J Rheumatol. 1992. 19:370–372.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Case of Bilateral Internuclear Ophthalmoplegia
- Extensive Longitudinal Myelitis Associated with Systemic Lupus Erythematosus: A case report
- A Case of Transverse Myelitis associated with Systemic Lupus Erythematosus
- A Case of Systemic Lupus Erythematosus with Recurrent Myelitis and Optic Neuritis