Korean J Radiol.
2015 Aug;16(4):942-946. 10.3348/kjr.2015.16.4.942.
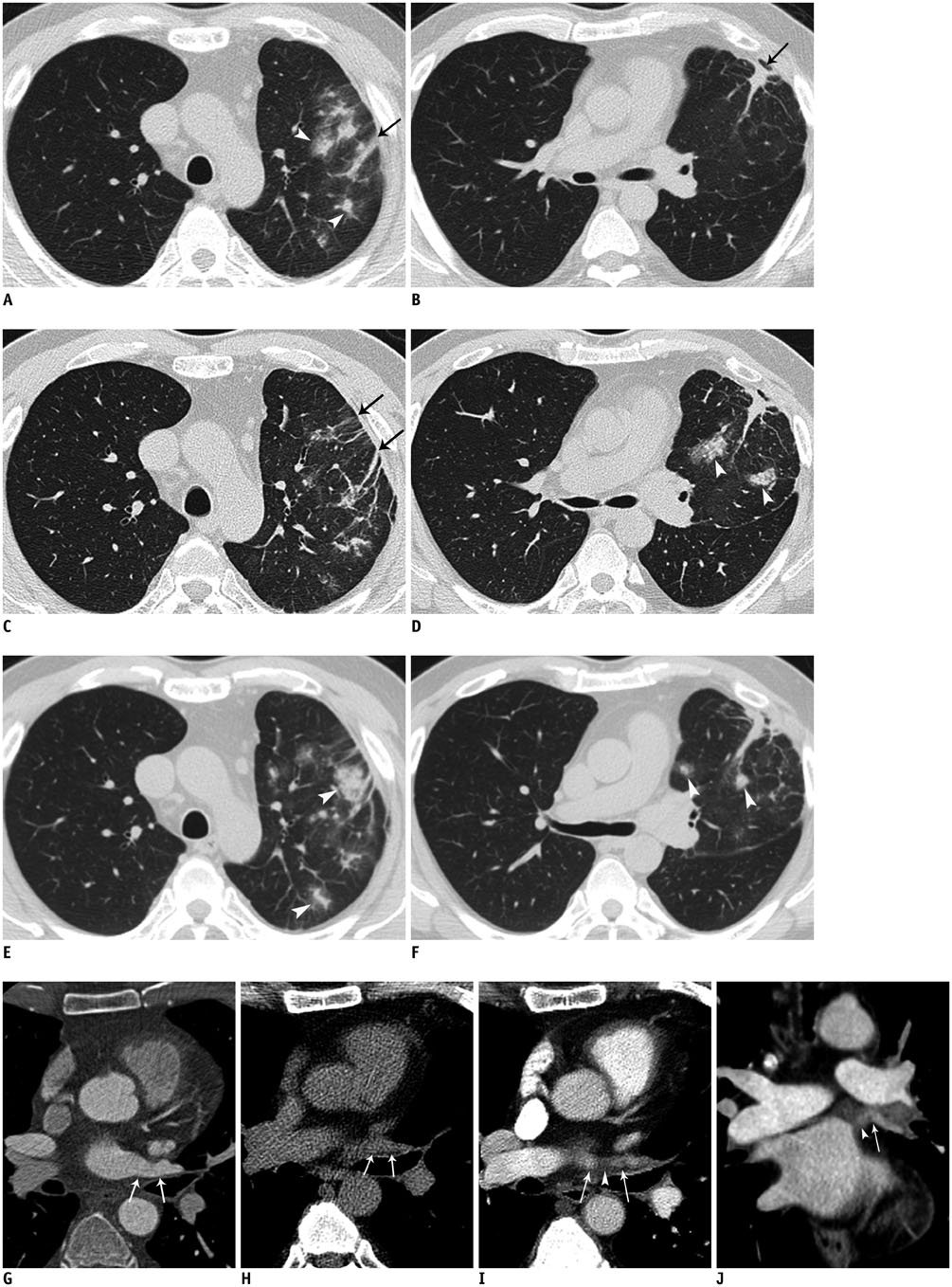
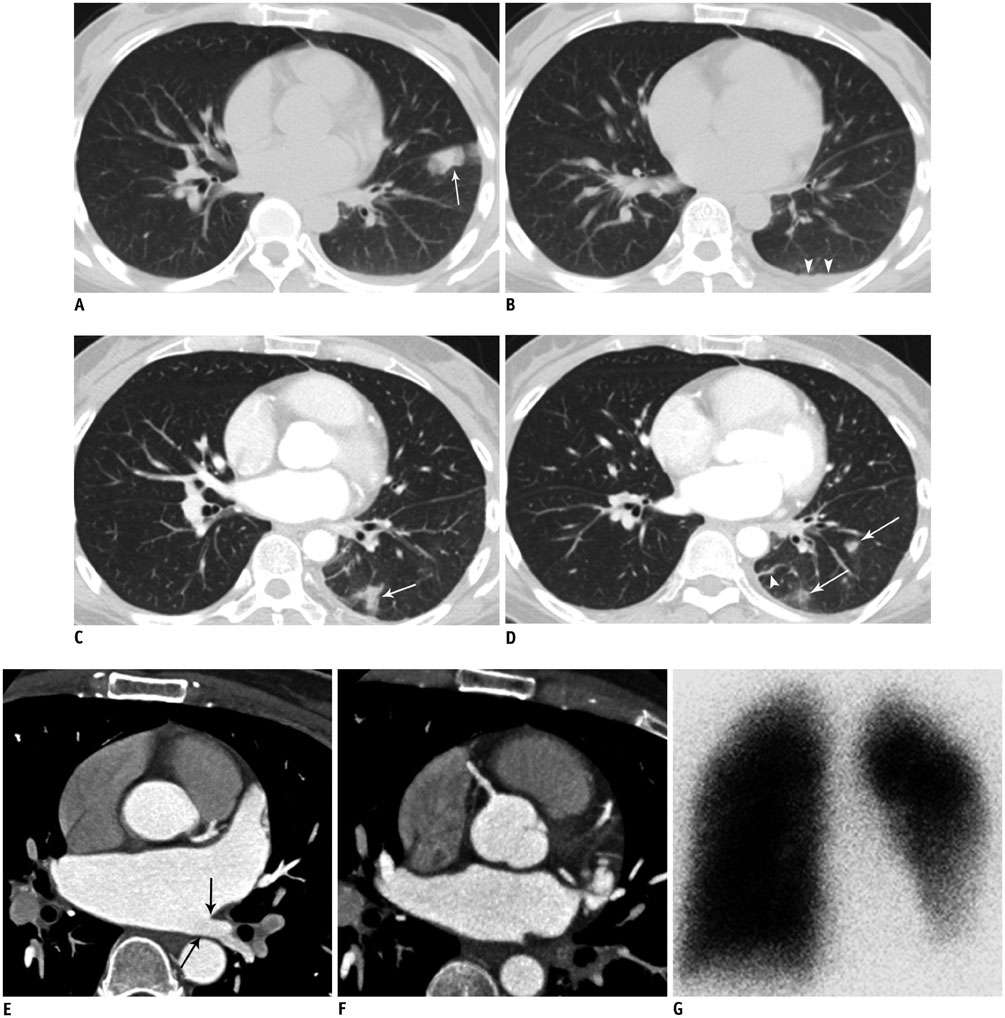
Lung Infarction due to Pulmonary Vein Stenosis after Ablation Therapy for Atrial Fibrillation Misdiagnosed as Organizing Pneumonia: Sequential Changes on CT in Two Cases
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. hoyunlee96@gmail.com
- 2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- 3Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- KMID: 2155571
- DOI: http://doi.org/10.3348/kjr.2015.16.4.942
Abstract
- Pulmonary vein (PV) stenosis is a complication of ablation therapy for arrhythmias. We report two cases with chronic lung parenchymal abnormalities showing no improvement and waxing and waning features, which were initially diagnosed as nonspecific pneumonias, and finally confirmed as PV stenosis. When a patient presents for nonspecific respiratory symptoms without evidence of infection after ablation therapy and image findings show chronic and repetitive parenchymal abnormalities confined in localized portion, the possibility of PV stenosis should be considered.
Keyword
MeSH Terms
-
Atrial Fibrillation/surgery
Catheter Ablation/*adverse effects/methods
Constriction, Pathologic/diagnosis/*radiography
*Diagnostic Errors
Female
Humans
Lung/surgery
Male
Middle Aged
Pneumonia/diagnosis
Pulmonary Infarction/pathology/*radiography
Pulmonary Veins/physiopathology/radiography
Tomography, X-Ray Computed/adverse effects
Vascular Diseases/physiopathology
Figure
Reference
-
1. Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998; 339:659–666.2. Packer DL, Keelan P, Munger TM, Breen JF, Asirvatham S, Peterson LA, et al. Clinical presentation, investigation, and management of pulmonary vein stenosis complicating ablation for atrial fibrillation. Circulation. 2005; 111:546–554.3. Ravenel JG, McAdams HP. Pulmonary venous infarction after radiofrequency ablation for atrial fibrillation. AJR Am J Roentgenol. 2002; 178:664–666.4. Yataco J, Stoller JK. Pulmonary venous thrombosis and infarction complicating pulmonary venous stenosis following radiofrequency ablation. Respir Care. 2004; 49:1525–1527.5. Chen SA, Hsieh MH, Tai CT, Tsai CF, Prakash VS, Yu WC, et al. Initiation of atrial fibrillation by ectopic beats originating from the pulmonary veins: electrophysiological characteristics, pharmacological responses, and effects of radiofrequency ablation. Circulation. 1999; 100:1879–1886.6. Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005; 111:1100–1105.7. Ernst S, Ouyang F, Goya M, Löber F, Schneider C, Hoffmann-Riem M, et al. Total pulmonary vein occlusion as a consequence of catheter ablation for atrial fibrillation mimicking primary lung disease. J Cardiovasc Electrophysiol. 2003; 14:366–370.8. Williamson WA, Tronic BS, Levitan N, Webb-Johnson DC, Shahian DM, Ellis FH Jr. Pulmonary venous infarction. Chest. 1992; 102:937–940.9. Pürerfellner H, Aichinger J, Martinek M, Nesser HJ, Cihal R, Gschwendtner M, et al. Incidence, management, and outcome in significant pulmonary vein stenosis complicating ablation for atrial fibrillation. Am J Cardiol. 2004; 93:1428–1431. A1010. Holmes DR Jr, Monahan KH, Packer D. Pulmonary vein stenosis complicating ablation for atrial fibrillation: clinical spectrum and interventional considerations. JACC Cardiovasc Interv. 2009; 2:267–276.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Controlled Atrial Fibrillation after Pulmonary Vein Stenting
- Lobectomy due to Pulmonary Vein Occlusion after Radiofrequency Ablation for Atrial Fibrillation
- Percutaneous Pulmonary Vein Angioplasty for the Pulmonary Vein Stenosis After Catheter Ablation of Atrial Fibrillation
- How to Achieve Complete and Permanent Pulmonary Vein Isolation without Complications
- Non-medication Treatment of Atrial Fibrillation