Korean J Radiol.
2015 Aug;16(4):860-865. 10.3348/kjr.2015.16.4.860.
Fluoroscopy-Guided Lumbar Drainage of Cerebrospinal Fluid for Patients in Whom a Blind Beside Approach Is Difficult
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam 463-707, Korea. netty0523@gmail.com
- KMID: 2155560
- DOI: http://doi.org/10.3348/kjr.2015.16.4.860
Abstract
OBJECTIVE
To evaluate the rates of technical success, clinical success, and complications of fluoroscopy-guided lumbar cerebrospinal fluid drainage.
MATERIALS AND METHODS
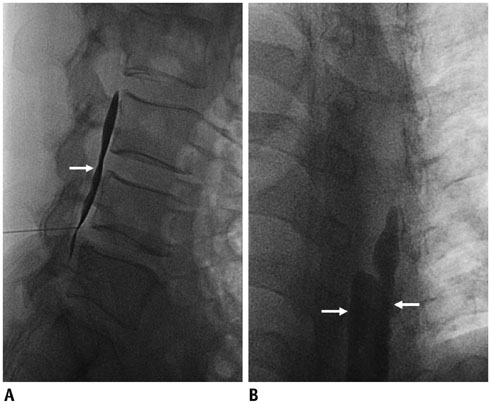
This retrospective study was approved by the Institutional Review Board of our hospital, and informed consent was waived. Ninety-six procedures on 60 consecutive patients performed July 2008 to December 2013 were evaluated. The patients were referred for the fluoroscopy-guided procedure due to failed attempts at a bedside approach, a history of lumbar surgery, difficulty cooperating, or obesity. Fluoroscopy-guided lumbar drainage procedures were performed in the lateral decubitus position with a midline puncture of L3/4 in the interspinous space. The catheter tip was positioned at the T12/L1 level, and the catheter was visualized on contrast agent-aided fluoroscopy. A standard angiography system with a rotatable C-arm was used. The definitions of technical success, clinical success, and complications were defined prior to the study.
RESULTS
The technical and clinical success rates were 99.0% (95/96) and 89.6% (86/96), respectively. The mean hospital stay for an external lumbar drain was 4.84 days. Nine cases of minor complications and eight major complications were observed, including seven cases of meningitis, and one retained catheter requiring surgical removal.
CONCLUSION
Fluoroscopy-guided external lumbar drainage is a technically reliable procedure in difficult patients with failed attempts at a bedside procedure, history of lumbar surgery, difficulties in cooperation, or obesity.
Keyword
MeSH Terms
Figure
Reference
-
1. Findler G, Sahar A, Beller AJ. Continuous lumbar drainage of cerebrospinal fluid in neurosurgical patients. Surg Neurol. 1977; 8:455–457.2. Post KD, Stein BM. Technique for spinal drainage. Neurosurgery. 1979; 4:255.3. Roland PS, Marple BF, Meyerhoff WL, Mickey B. Complications of lumbar spinal fluid drainage. Otolaryngol Head Neck Surg. 1992; 107:564–569.4. Gold MM, Miller TS, Farinhas JM, Altschul DJ, Bello JA, Brook AL. Computed tomography-guided lumbar drain placement. J Neurosurg Spine. 2008; 9:372–373.5. Eskey CJ, Ogilvy CS. Fluoroscopy-guided lumbar puncture: decreased frequency of traumatic tap and implications for the assessment of CT-negative acute subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2001; 22:571–576.6. Brook AD, Burns J, Dauer E, Schoendfeld AH, Miller TS. Comparison of CT and fluoroscopic guidance for lumbar puncture in an obese population with prior failed unguided attempt. J Neurointerv Surg. 2014; 6:324–328.7. Sato K, Shimizu S, Oka H, Fujii K. Intraoperative fluoroscopy with contrast medium for correct lumbar catheter placement in lumboperitoneal shunts. Kitasato Med J. 2013; 43:155–158.8. Graf CJ, Gross CE, Beck DW. Complications of spinal drainage in the management of cerebrospinal fluid fistula. J Neurosurg. 1981; 54:392–395.9. Kitchel SH, Eismont FJ, Green BA. Closed subarachnoid drainage for management of cerebrospinal fluid leakage after an operation on the spine. J Bone Joint Surg Am. 1989; 71:984–987.10. Shapiro SA, Scully T. Closed continuous drainage of cerebrospinal fluid via a lumbar subarachnoid catheter for treatment or prevention of cranial/spinal cerebrospinal fluid fistula. Neurosurgery. 1992; 30:241–245.11. Açikbaş SC, Akyüz M, Kazan S, Tuncer R. Complications of closed continuous lumbar drainage of cerebrospinal fluid. Acta Neurochir (Wien). 2002; 144:475–480.12. Coplin WM, Avellino AM, Kim DK, Winn HR, Grady MS. Bacterial meningitis associated with lumbar drains: a retrospective cohort study. J Neurol Neurosurg Psychiatry. 1999; 67:468–473.13. Governale LS, Fein N, Logsdon J, Black PM. Techniques and complications of external lumbar drainage for normal pressure hydrocephalus. Neurosurgery. 2008; 63:4 Suppl 2. 379–384. discussion 38414. Farhat HI, Elhammady MS, Levi AD, Aziz-Sultan MA. Cervical subarachnoid catheter placement for continuous cerebrospinal fluid drainage: a safe and efficacious alternative to the classic lumbar cistern drain. Neurosurgery. 2011; 68:1 Suppl Operative. 52–56. discussion 56
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transvaginal Drainage of Pelvic Fluid Collections Unsuitable for Transabdominal Approach
- The evaluation of image-guided catheter drainage in pleural effusion and empyema
- Acquired Chiari Malformation
- Management of Persistent Cerebrospinal Fluid Leakage Following Thoraco-lumbar Surgery
- Ultrasound-Guided Intervention in Lumbar Spine