J Korean Med Sci.
2015 May;30(5):644-650. 10.3346/jkms.2015.30.5.644.
Inpatient Stroke Rehabilitation Outcomes in Korea Derived from the Korean Brain Rehabilitation Centers' Online Database System for the Years 2007 to 2011
- Affiliations
-
- 1Department of Physical & Rehabilitation Medicine, School of Medicine, Inha University, Incheon, Korea. rmjung@inha.ac.kr
- 2Department of Physical & Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Physical & Rehabilitation Medicine, Korea University School of Medicine, Seoul, Korea.
- 4Department of Physical & Rehabilitation Medicine, Ajou University College of Medicine, Suwon, Korea.
- 5Department of Physical & Rehabilitation Medicine, The Catholic University of Korea School of Medicine, Seoul, Korea.
- 6Department of Physical & Rehabilitation Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 7Department of Physical & Rehabilitation Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- 8Department of Physical & Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 9Department of Physical & Rehabilitation Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- 10Department of Physical & Rehabilitation Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 11Department of Physical & Rehabilitation Medicine, National Rehabilitation Center, Seoul, Korea.
- 12Department of Physical & Rehabilitation Medicine, The Catholic University of Korea School of Medicine, St. Vincent's Hospital, Suwon, Korea.
- KMID: 2155480
- DOI: http://doi.org/10.3346/jkms.2015.30.5.644
Abstract
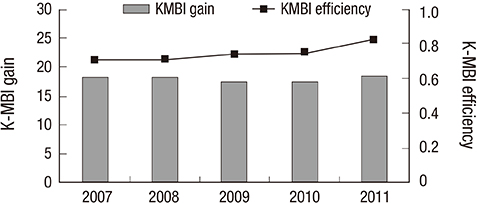
- The purpose of this report was to provide information for patients receiving inpatient rehabilitation after stroke and to identify the possible factors influencing functional outcome after inpatient rehabilitation. Stroke patients (n = 5,212) who were discharged from the Departments of Rehabilitation Medicine (RM) of university hospitals and rehabilitation hospitals from 2007 through 2011 were participants. Prevalence, age, transfer time after onset, length of stay (LOS), functional status at admission and discharge were analyzed. In all stroke subjects, cerebral infarctions (67%) were more common than hemorrhages. Cerebral infarctions in the middle cerebral artery territory were most common, while the basal ganglia and cerebral cortex were the most common areas for hemorrhagic stroke. The LOS decreased from 45 to 28 days. Transfer time after onset decreased from 44 to 30 days. Shorter transfer time after onset was correlated with better discharge functional status and shorter LOS. Initial functional status was correlated with discharge functional status. In ischemic stroke subtypes, cerebellar and brainstem strokes predicted better outcomes, while strokes with more than one territory predicted poorer outcomes with more disabilities. In hemorrhagic stroke subtypes, initial and discharge functional status was the lowest for cortical hemorrhages and highest for brainstem hemorrhages. This report shows that LOS and transfer time after onset has been decreased over time and initial functional status and shorter transfer after onset are predictors of better functional outcome at discharge.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Stroke Rehabilitation Fact Sheet in Korea
Se Hee Jung
Ann Rehabil Med. 2022;46(1):1-8. doi: 10.5535/arm.22001.
Reference
-
1. Yang SN, Park SW, Jung HY, Rah UW, Kim YH, Chun MH, Paik NJ, Yoo SD, Pyun SB, Kim MW, et al. Korean Brain Rehabilitation Registry for rehabilitation of persons with brain disorders: annual report in 2009. J Korean Med Sci. 2012; 27:691–696.2. Granger CV, Markello SJ, Graham JE, Deutsch A, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of patients with stroke discharged from comprehensive medical programs in 2000-2007. Am J Phys Med Rehabil. 2009; 88:961–972.3. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, Kim SH, Kim TH, Han TR. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.4. Choi SH, Na DL, Kwon HM, Yoon SJ, Jeong JH, Ha CK. The Korean version of the neuropsychiatric inventory: a scoring tool for neuropsychiatric disturbance in dementia patients. J Korean Med Sci. 2000; 15:609–615.5. Beninato M, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch Phys Med Rehabil. 2006; 87:32–39.6. Jackson C, Sudlow C. Comparing risks of death and recurrent vascular events between lacunar and non-lacunar infarction. Brain. 2005; 128:2507–2517.7. US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013; 310:591–608.8. Murakami M, Inouye M. Stroke rehabilitation outcome study: a comparison of Japan with the United States. Am J Phys Med Rehabil. 2002; 81:279–282.9. Shah S, Vanclay F, Cooper B. Predicting discharge status at commencement of stroke rehabilitation. Stroke. 1989; 20:766–769.10. Denti L, Agosti M, Franceschini M. Outcome predictors of rehabilitation for first stroke in the elderly. Eur J Phys Rehabil Med. 2008; 44:3–11.11. Oneş K, Yalçinkaya EY, Toklu BC, Cağlar N. Effects of age, gender, and cognitive, functional and motor status on functional outcomes of stroke rehabilitation. NeuroRehabilitation. 2009; 25:241–249.12. Hu MH, Hsu SS, Yip PK, Jeng JS, Wang YH. Early and intensive rehabilitation predicts good functional outcomes in patients admitted to the stroke intensive care unit. Disabil Rehabil. 2010; 32:1251–1259.13. Salter K, Jutai J, Hartley M, Foley N, Bhogal S, Bayona N, Teasell R. Impact of early vs delayed admission to rehabilitation on functional outcomes in persons with stroke. J Rehabil Med. 2006; 38:113–117.14. Maulden SA, Gassaway J, Horn SD, Smout RJ, DeJong G. Timing of initiation of rehabilitation after stroke. Arch Phys Med Rehabil. 2005; 86:S34–s40.15. Bhalla A, Wang Y, Rudd A, Wolfe CD. Differences in outcome and predictors between ischemic and intracerebral hemorrhage: the South London Stroke Register. Stroke. 2013; 44:2174–2181.16. Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, Fusco FR, Morelli D, Venturiero V, Troisi E, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke. 2003; 34:2861–2865.17. Cals N, Devuyst G, Afsar N, Karapanayiotides T, Bogousslavsky J. Pure superficial posterior cerebral artery territory infarction in The Lausanne Stroke Registry. J Neurol. 2002; 249:855–861.18. Kumral E, Bayulkem G, Evyapan D, Yunten N. Spectrum of anterior cerebral artery territory infarction: clinical and MRI findings. Eur J Neurol. 2002; 9:615–624.19. Heinsius T, Bogousslavsky J, Van Melle G. Large infarcts in the middle cerebral artery territory. Etiology and outcome patterns. Neurology. 1998; 50:341–350.20. Kelly PJ, Stein J, Shafqat S, Eskey C, Doherty D, Chang Y, Kurina A, Furie KL. Functional recovery after rehabilitation for cerebellar stroke. Stroke. 2001; 32:530–534.21. Ng YS, Stein J, Ning M, Black-Schaffer RM. Comparison of clinical characteristics and functional outcomes of ischemic stroke in different vascular territories. Stroke. 2007; 38:2309–2314.22. Lindgren A, Norrving B, Rudling O, Johansson BB. Comparison of clinical and neuroradiological findings in first-ever stroke. A population-based study. Stroke. 1994; 25:1371–1377.23. Takeuchi S, Suzuki G, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yatsushige H, Shigeta K, Momose T, Wada K, et al. Prognostic factors in patients with primary brainstem hemorrhage. Clin Neurol Neurosurg. 2013; 115:732–735.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Inpatient Stroke Rehabilitation Outcomes in Korea Derived from the Korean Brain Rehabilitation Centers' Online Database System for the Years 2007 to 2011
- Changes in Epidemiological Trends and Rehabilitation Usage in Neurological Diseases in Korea: Stroke
- Stroke Rehabilitation Fact Sheet in Korea
- Launching of the accreditation system for rehabilitation facility in Korea
- Integrating Cardiac Rehabilitation with Neurorehabilitation in a Patient with Ischemic Stroke after Cardiac Surgery: a Case Report