J Korean Med Sci.
2015 Jan;30(1):104-109. 10.3346/jkms.2015.30.1.104.
The Scene Time Interval and Basic Life Support Termination of Resuscitation Rule in Adult Out-of-Hospital Cardiac Arrest
- Affiliations
-
- 1Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea.
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. shinsangdo@medimail.co.kr
- 3Department of Emergency Medicine, Inje University College of Medicine, Seoul, Korea.
- KMID: 2155454
- DOI: http://doi.org/10.3346/jkms.2015.30.1.104
Abstract
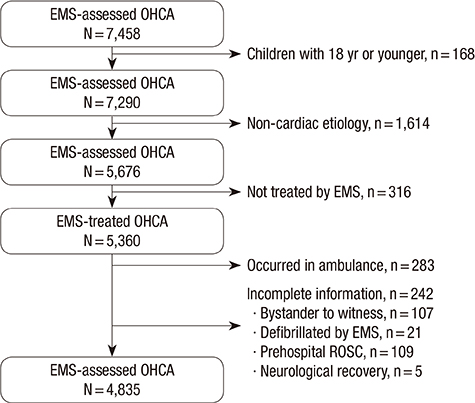
- We validated the basic life support termination of resuscitation (BLS TOR) rule retrospectively using Out-of-Hospital Cardiac Arrest (OHCA) data of metropolitan emergency medical service (EMS) in Korea. We also tested it by investigating the scene time interval for supplementing the BLS TOR rule. OHCA database of Seoul (January 2011 to December 2012) was used, which is composed of ambulance data and hospital medical record review. EMS-treated OHCA and 19 yr or older victims were enrolled, after excluding cases occurred in the ambulance and with incomplete information. The primary and secondary outcomes were hospital mortality and poor neurologic outcome. After calculating the sensitivity (SS), specificity (SP), and the positive and negative predictive values (PPV and NPV), tested the rule according to the scene time interval group for sensitivity analysis. Of total 4,835 analyzed patients, 3,361 (69.5%) cases met all 3 criteria of the BLS TOR rule. Of these, 3,224 (95.9%) were dead at discharge (SS,73.5%; SP,69.6%; PPV,95.9%; NPV, 21.3%) and 3,342 (99.4%) showed poor neurologic outcome at discharge (SS, 75.2%; SP, 89.9%; PPV, 99.4%; NPV, 11.5%). The cut-off scene time intervals for 100% SS and PPV were more than 20 min for survival to discharge and more than 14 min for good neurological recovery. The BLS TOR rule showed relatively lower SS and PPV in OHCA data in Seoul, Korea.
MeSH Terms
-
Adult
Advanced Cardiac Life Support/*mortality
Cardiopulmonary Resuscitation/*mortality
Critical Care/statistics & numerical data
Decision Support Techniques
Electric Countershock/*mortality
Emergency Medical Services
Female
Hospital Mortality
Humans
Male
Out-of-Hospital Cardiac Arrest/*epidemiology/*mortality/therapy
Refusal to Treat
Republic of Korea/epidemiology
Retrospective Studies
Survival Rate
Time Factors
Time-to-Treatment
Treatment Outcome
Figure
Cited by 1 articles
-
The Effect of Transport Time Interval on Neurological Recovery after Out-of-Hospital Cardiac Arrest in Patients without a Prehospital Return of Spontaneous Circulation
Jeong Ho Park, Yu Jin Kim, Young Sun Ro, Sola Kim, Won Chul Cha, Sang Do Shin
J Korean Med Sci. 2019;34(9):. doi: 10.3346/jkms.2019.34.e73.
Reference
-
1. Stiell IG, Wells GA, Spaite DW, Nichol G, O'Brien B, Munkley DP, Field BJ, Lyver MB, Luinstra LG, Dagnone E, et al. OPALS Study Group. The Ontario Prehospital Advanced Life Support (OPALS) study Part II: Rationale and methodology for trauma and respiratory distress patients. Ann Emerg Med. 1999; 34:256–262.2. Finlay I, Dallimore D. Your child is dead. BMJ. 1991; 302:1524–1525.3. Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehosp Emerg Care. 2001; 5:261–269.4. Morrison LJ, Kierzek G, Diekema DS, Sayre MR, Silvers SM, Idris AH, Mancini ME. Part 3: ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122:S665–S675.5. Verbeek PR, Vermeulen MJ, Ali FH, Messenger DW, Summers J, Morrison LJ. Derivation of a termination-of-resuscitation guideline for emergency medical technicians using automated external defibrillators. Acad Emerg Med. 2002; 9:671–678.6. Richman PB, Vadeboncoeur TF, Chikani V, Clark L, Bobrow BJ. Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med. 2008; 15:517–521.7. Morrison LJ, Verbeek PR, Zhan C, Kiss A, Allan KS. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009; 80:324–328.8. Ong ME, Jaffey J, Stiell I, Nesbitt L. OPALS Study Group. Comparison of termination-of-resuscitation guidelines for basic life support: defibrillator providers in out-of-hospital cardiac arrest. Ann Emerg Med. 2006; 47:337–343.9. Sasson C, Hegg AJ, Macy M, Park A, Kellermann A, McNally B. CARES Surveillance Group. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008; 300:1432–1438.10. Ruygrok ML, Byyny RL, Haukoos JS. Colorado Cardiac Arrest & Resuscitation Collaborative Study Group. Denver Metro EMS Medical Directors. Validation of 3 termination of resuscitation criteria for good neurologic survival after out-of-hospital cardiac arrest. Ann Emerg Med. 2009; 54:239–247.11. Skrifvars MB, Vayrynen T, Kuisma M, Castren M, Parr MJ, Silfverstople J, Svensson L, Jonsson L, Herlitz J. Comparison of Helsinki and European Resuscitation Council "do not attempt to resuscitate" guidelines, and a termination of resuscitation clinical prediction rule for out-of-hospital cardiac arrest patients found in asystole or pulseless electrical activity. Resuscitation. 2010; 81:679–684.12. Morrison LJ, Visentin LM, Kiss A, Theriault R, Eby D, Vermeulen M, Sherbino J, Verbeek PR. TOR Investigators. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006; 355:478–487.13. Shin SD, Ong ME, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, Karim SA, Khunkhlai N, Lin CH, Song KJ, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care. 2012; 16:477–496.14. Petrie DA, De Maio V, Stiell IG, Dreyer J, Martin M, O'Brien JA. Factors affecting survival after prehospital asystolic cardiac arrest in a Basic Life Support-Defibrillation system. CJEM. 2001; 3:186–192.15. Marsden AK, Ng GA, Dalziel K, Cobbe SM. When is it futile for ambulance personnel to initiate cardiopulmonary resuscitation? BMJ. 1995; 311:49–51.16. Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990; 112:949–954.17. Mohr M, Bahr J, Schmid J, Panzer W, Kettler D. The decision to terminate resuscitative efforts: results of a questionnaire. Resuscitation. 1997; 34:51–55.18. Zive D, Koprowicz K, Schmidt T, Stiell I, Sears G, Van Ottingham L, Idris A, Stephens S, Daya M. Resuscitation Outcomes Consortium Investigators. Variation in out-of-hospital cardiac arrest resuscitation and transport practices in the Resuscitation Outcomes Consortium: ROC Epistry-Cardiac Arrest. Resuscitation. 2011; 82:277–284.19. Ong ME, Tan EH, Ng FS, Yap S, Panchalingham A, Leong BS, Ong VY, Tiah L, Lim SH, Venkataraman A, et al. Comparison of termination-of-resuscitation guidelines for out-of-hospital cardiac arrest in Singapore EMS. Resuscitation. 2007; 75:244–251.20. Kajino K, Kitamura T, Iwami T, Daya M, Ong ME, Hiraide A, Shimazu T, Kishi M, Yamayoshi S. Current termination of resuscitation (TOR) guidelines predict neurologically favorable outcome in Japan. Resuscitation. 2013; 84:54–59.21. Shin SD, Kitamura T, Hwang SS, Kajino K, Song KJ, Ro YS, Nishiuchi T, Iwami T. Seoul-Osaka Resuscitation Study (SORS) Group. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014; 85:203–210.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Guideline of Pediatric Cardiopulmonary Resuscitation
- Analysis of reasons for the termination of resuscitation in non-traumatic out-of-hospital cardiac arrests before and after the COVID-19 pandemic
- Validation of Termination Guidelines for Out of Hospital Cardiac Arrest in Korea
- Cardiopulmonary Resuscitation: New Concept
- Application of a Dual-Dispatch System for Out-of-Hospital Cardiac Arrest Patients: Will More Hands Save More Lives?