Ann Surg Treat Res.
2016 Mar;90(3):164-170. 10.4174/astr.2016.90.3.164.
The feasibility of single-port laparoscopic appendectomy using a solo approach: a comparative study
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea. zambo9@catholic.ac.kr
- KMID: 2155050
- DOI: http://doi.org/10.4174/astr.2016.90.3.164
Abstract
- PURPOSE
To investigate the feasibility and safety of solo surgery with single-port laparoscopic appendectomy, which is termed herein solo-SPLA (solo-single-port laparoscopic appendectomy).
METHODS
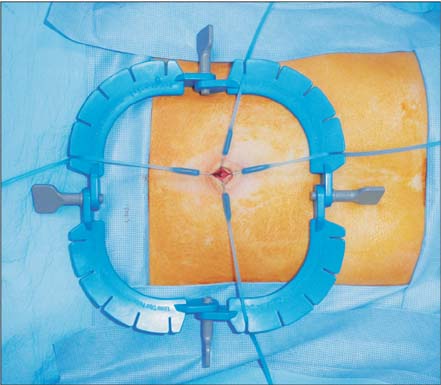
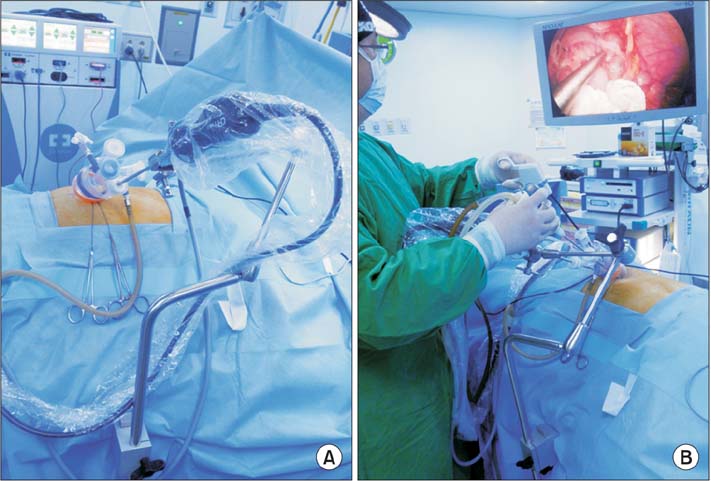
This study prospectively collected and retrospectively analyzed data from patients who had undergone either non-solo-SPLA (n = 150) or solo-SPLA (n = 150). Several devices were utilized for complete, skin-to-skin solo-SPSA, including a Lone Star Retractor System and an adjustable mechanical camera holder.
RESULTS
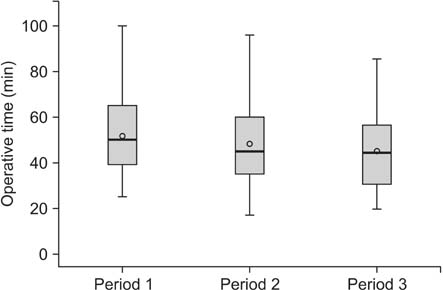
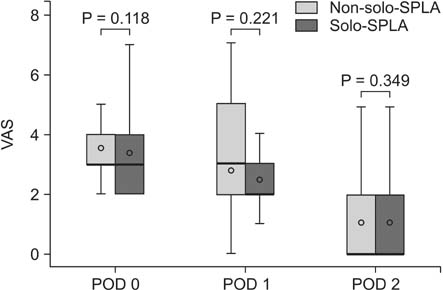
Operating times were not significantly different between solo- and non-solo-SPLA (45.0 +/- 21.0 minutes vs. 46.7 +/- 26.1 minutes, P = 0.646). Most postoperative variables were also comparable between groups, including the necessity for intravenous analgesics (0.7 +/- 1.2 ampules [solo-SPLA] vs. 0.9 +/- 1.5 ampules [non-solo-SPLA], P = 0.092), time interval to gas passing (1.3 +/- 1.0 days vs. 1.4 +/- 1.0 days, P = 0.182), and the incidence of postoperative complications (4.0% vs. 8.7%, P = 0.153). Moreover, solo-SPLA effectively lowered the operating cost by reducing surgical personnel expenses.
CONCLUSION
Solo-SPLA economized staff numbers and thus lowered hospital costs without lengthening of operating time. Therefore, solo-SPLA could be considered a safe and feasible alternative to non-solo-SPLA.
MeSH Terms
Figure
Cited by 1 articles
-
Comparing the short-term outcomes and cost between solo single-incision distal gastrectomy and conventional multiport totally laparoscopic distal gastrectomy for early gastric cancer: a propensity score-matched analysis
Boram Lee, Sang Il Youn, Kanghaeng Lee, Yongjoon Won, Sahong Min, Yoon Taek Lee, Young Suk Park, Sang-Hoon Ahn, Do Joong Park, Hyung-Ho Kim
Ann Surg Treat Res. 2021;100(2):67-75. doi: 10.4174/astr.2021.100.2.67.
Reference
-
1. Arezzo A, Ulmer F, Weiss O, Schurr MO, Hamad M, Buess GF. Experimental trial on solo surgery for minimally invasive therapy: comparison of different systems in a phantom model. Surg Endosc. 2000; 14:955–959.2. Schurr MO, Buess GF. Systems technology in the operating theatre: a prerequisite for the use of advanced devices in surgery. Minim Invasive Ther Allied Technol. 2000; 9:179–184.3. Kim SJ, Lee SC. Technical and instrumental prerequisites for single-port laparoscopic solo surgery: state of art. World J Gastroenterol. 2015; 21:4440–4446.4. Chen YC, Shih CL, Wu CH, Chiu CH. Exploring factors that have caused a decrease in surgical manpower in Taiwan. Surg Innov. 2014; 21:520–527.5. Deedar-Ali-Khawaja R, Khan SM. Trends of surgical career selection among medical students and graduates: a global perspective. J Surg Educ. 2010; 67:237–248.6. Marschall JG, Karimuddin AA. Decline in popularity of general surgery as a career choice in North America: review of postgraduate residency training selection in Canada, 1996-2001. World J Surg. 2003; 27:249–252.7. Kronberg U, Kiran RP, Soliman MS, Hammel JP, Galway U, Coffey JC, et al. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg. 2011; 253:78–81.8. Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, et al. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011; 254:933–940.9. Biondi A, Grosso G, Mistretta A, Marventano S, Toscano C, Drago F, et al. Laparoscopic vs. open approach for colorectal cancer: evolution over time of minimal invasive surgery. BMC Surg. 2013; 13:Suppl 2. S12.10. Shoemaker P, Schuhmann TM. Trends in hospitals' use of contract labor. Healthc Financ Manage. 2007; 61:70–74.11. Gillen S, Pletzer B, Heiligensetzer A, Wolf P, Kleeff J, Feussner H, et al. Solo-surgical laparoscopic cholecystectomy with a joystick-guided camera device: a case-control study. Surg Endosc. 2014; 28:164–170.12. den Boer KT, Bruijn M, Jaspers JE, Stassen LP, Erp WF, Jansen A, et al. Time-action analysis of instrument positioners in laparoscopic cholecystectomy. Surg Endosc. 2002; 16:142–147.13. Voorhorst FA, Meijer DW, Overbeeke CJ. Head-controlled laparoscopy: experiment, prototype, and preliminary results. J Laparoendosc Adv Surg Tech A. 1999; 9:379–388.14. Hollander SW, Klingen HJ, Fritz M, Djalali P, Birk D. Robotic camera assistance and its benefit in 1033 traditional laparoscopic procedures: prospective clinical trial using a joystick-guided camera holder. Surg Technol Int. 2014; 25:19–23.15. Gaujoux S, Bretagnol F, Au J, Ferron M, Panis Y. Single port access proctectomy with total mesorectal excision and intersphincteric resection with a primary transanal approach. Colorectal Dis. 2011; 13:e305–e307.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feasibility of Single-Incision Laparoscopic Appendectomy in Pregnant Women
- Single-Port Laparoscopic Solo Surgery: Technical Aspects and Personal Experience
- Single-Port Laparoscopic Appendectomy
- Single Port Laparoscopic Appendectomy: Retrospective and Comparative Analysis of 55 Consecutive Cases: Report of Initial Experience
- Solo Single-Incision Laparoscopic Appendectomy versus Conventional Single-Incision Laparoscopic Appendectomy: A Retrospective, Single Center Study