Neurointervention.
2015 Sep;10(2):82-88. 10.5469/neuroint.2015.10.2.82.
Enlarged Parent Artery Lumen at Aneurysmal-Neck Segment in Wide-Necked Distal Internal Carotid Artery Aneurysms
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, Seoul, Korea. dhlee@amc.seoul.kr
- 2Department of Medicine, University of Ulsan College of Medicine, Ulsan, Korea.
- 3Department of Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 4Angiovention, Gyeonggi-do, Korea.
- KMID: 2148998
- DOI: http://doi.org/10.5469/neuroint.2015.10.2.82
Abstract
- PURPOSE
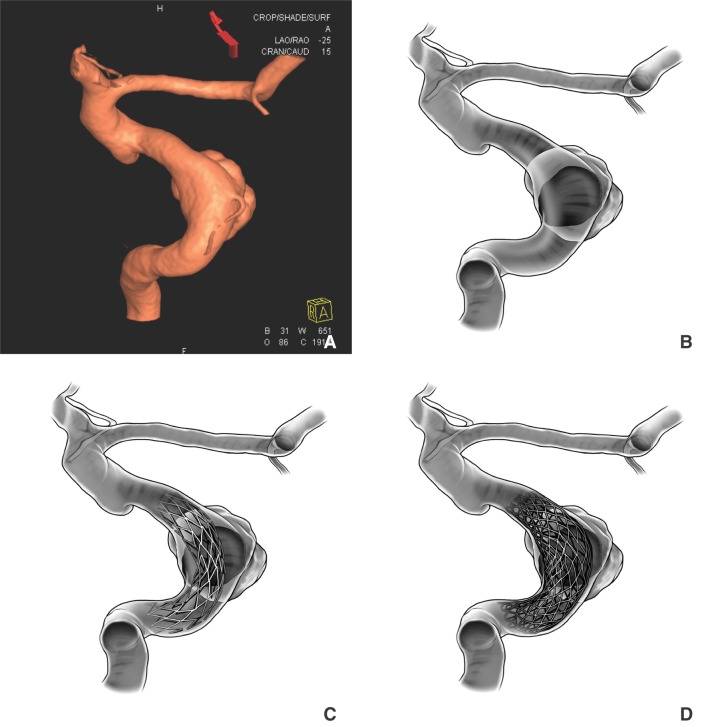
Hypothesizing that the parent artery (PA) diameter of the aneurysm-neck segment is larger than those of normal segments, especially in wide-necked aneurysm cases, we conducted 3D angiographic analyses in wide-necked aneurysm cases focusing on the luminal morphologic change of the PA.
MATERIALS AND METHODS
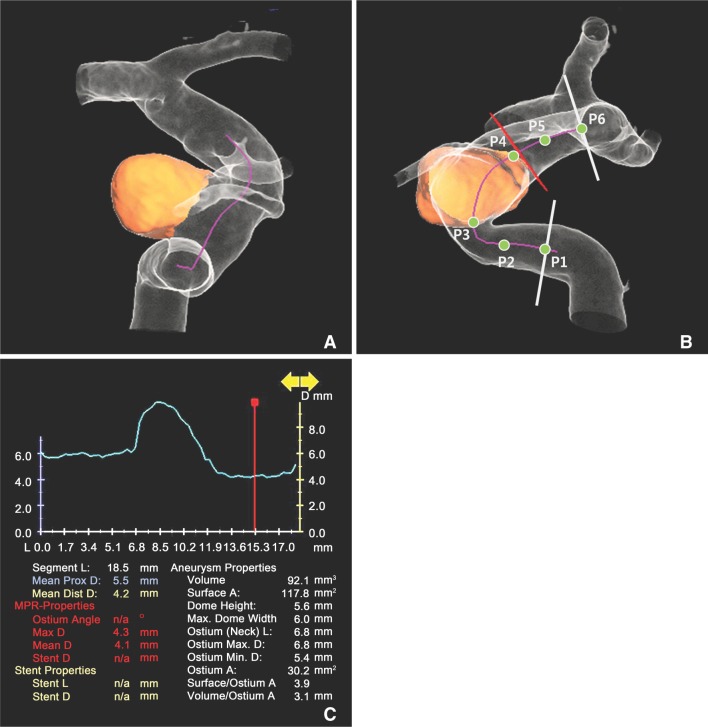
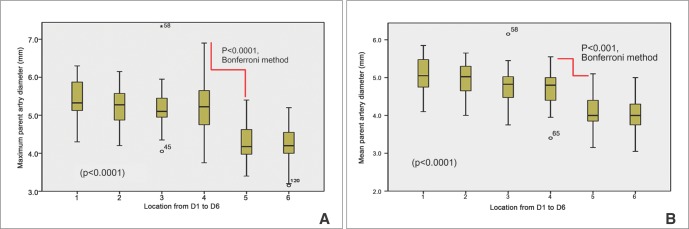
Under the approval of local IRB, we enrolled 26 patients with distal internal carotid artery (ICA) aneurysms, which were treated with stent assisted coiling. The PA diameters along the centerline were measured at 6 points with built-in software by two observers. Those 6 points were P1 and P2 proximally, P3 and P4 at the aneurysm ostium margins, and P5 and P6 distally. We performed an ANOVA test and a Bonferroni method for post hoc analyses. Linear regression analysis was performed to find any morphologic influencing factors.
RESULTS
There were 20 distal ICA aneurysms out of 26 consecutive cases after exclusion. The differences in diameter at each point were statistically significant (p<0.0001). On post hoc analyses, the difference between P4 and P5 was significant both in maximum and mean PA diameters (p<0.0001 and p<0.001, respectively). Multivariate analyses failed to reveal any morphological influencing factor.
CONCLUSION
PAs harboring a wide-necked aneurysm requiring stent assistance for coiling showed significant enlargement of the lumen, especially at the distal transition segment of the aneurysm ostium and the PA.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Alpha Stent for Coiling of Unruptured, Wide-Necked, Distal Internal Carotid Artery Aneurysms: Safety and Effectiveness at 6 Months
Yunsun Song, Jae Jon Sheen, Joong-Goo Kim, Sang Hun Lee, Su Hee Cho, Jung Cheol Park, Choong Gon Choi, Deok Hee Lee
Korean J Radiol. 2020;21(2):228-235. doi: 10.3348/kjr.2019.0188.In Vitro Evaluation of Fusiform-Shaped Stents for Wide-Neck Intracranial Aneurysm Treatment
Zhen Yu Jia, Yuan Yuan Jiang, Jung Min Woo, Seon Moon Hwang, Ok Kyun Lim, Tae Il Kim, Jung Cheol Park, Hee Sun Lee, Eun Sang Kim, Deok Hee Lee
Neurointervention. 2018;13(2):117-123. doi: 10.5469/neuroint.2018.00976.
Reference
-
1. Lesley WS, Patel DV. Neuroform-EZ Stent Modification for Facilitated Delivery during Intracranial Aneurysm Embosurgery. Neurointervention. 2013; 8:101–104. PMID: 24024074.
Article2. Heller RS, Malek AM. Delivery technique plays an important role in determining vessel wall apposition of the enterprise selfexpanding intracranial stent. J Neurointerv Surg. 2011; 3:340–343. PMID: 21990459.
Article3. Turk AS, Strother CM, Crouthamel DI, Zagzebski JA. Definition of the ostium (neck) of an aneurysm revealed by intravascular sonography: an experimental study in canines. AJNR Am J Neuroradiol. 1999; 20:1301–1308. PMID: 10472990.4. Yasuda R, Arat A, Strother CM, Aagaard-Kienitz B, Niemann D, Mohamed A, et al. Aneurysm ostium angle: a predictor of the need for stent as assistance for endovascular aneurysm coiling in internal carotid artery sidewall aneurysms. AJNR Am J Neuroradiol. 2011; 32:1216–1220. PMID: 21700791.
Article5. Lasjaunias PL. Segmental identity and vulnerability in cerebral arteries. Interv Neuroradiol. 2000; 6:113–124. PMID: 20667189.
Article6. Farnoush A, Qian Y, Takao H, Murayama Y, Avolio A. Effect of saccular aneurysm and parent artery morphology on hemodynamics of cerebral bifurcation aneurysms. Conf Proc IEEE Eng Med Biol Soc. 2012; 2012:6677–6680. PMID: 23367461.
Article7. Krischek O, Miloslavski E, Fischer S, Shrivastava S, Henkes H. A comparison of functional and physical properties of self-expanding intracranial stents [Neuroform3, Wingspan, Solitaire, Leo+, Enterprise]. Minim Invasive Neurosurg. 2011; 54:21–28. PMID: 21506064.
Article8. Heller RS, Miele WR, Do-Dai DD, Malek AM. Crescent sign on magnetic resonance angiography revealing incomplete stent apposition: correlation with diffusion-weighted changes in stentmediated coil embolization of aneurysms. J Neurosurg. 2011; 115:624–632. PMID: 21619405.
Article9. Ding D, Starke RM, Durst CR, Gaughen JR Jr, Evans AJ, Jensen ME, et al. Dynact imaging for intraprocedural evaluation of flowdiverting stent apposition during endovascular treatment of intracranial aneurysms. J Clin Neurosci. 2014; 21:1981–1983. PMID: 24856039.
Article10. Matsumura JS, Gray W, Chaturvedi S, Yamanouchi D, Peng L, Verta P. Results of carotid artery stenting with distal embolic protection with improved systems: Protected Carotid Artery Stenting in Patients at High Risk for Carotid Endarterectomy (PROTECT) trial. J Vasc Surg. 2012; 55:968–976. PMID: 22236885.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of "Double-catheter" Technique in GDC Treatment of Intracranial Wide-necked Aneurysm
- Comparison of CT Angiography and Digital Subtraction Angiography in the Evaluation of Intracranial Aneurysmal Neck
- Kinking of Flow Diverter in a Giant Wide-Necked Supraclinoid Internal Carotid Artery Aneurysm
- Multiple Clipping Technique of Wide-Necked Middle Cerebral Artery Aneurysms
- Microcatheter-assisted Coil Embolization of Distal Vertebral Artery Wide-Necked Aneurysm: A Case Report