J Korean Ophthalmol Soc.
2015 Jul;56(7):1075-1080. 10.3341/jkos.2015.56.7.1075.
Treatment Outcome of Triple Procedure in Open-Angle Glaucoma and Angle-Closure Glaucoma
- Affiliations
-
- 1The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. kcyeye@yuhs.ac
- KMID: 2148808
- DOI: http://doi.org/10.3341/jkos.2015.56.7.1075
Abstract
- PURPOSE
To compare the surgical outcomes of triple procedure in patients with open-angle glaucoma and angle-closure glaucoma.
METHODS
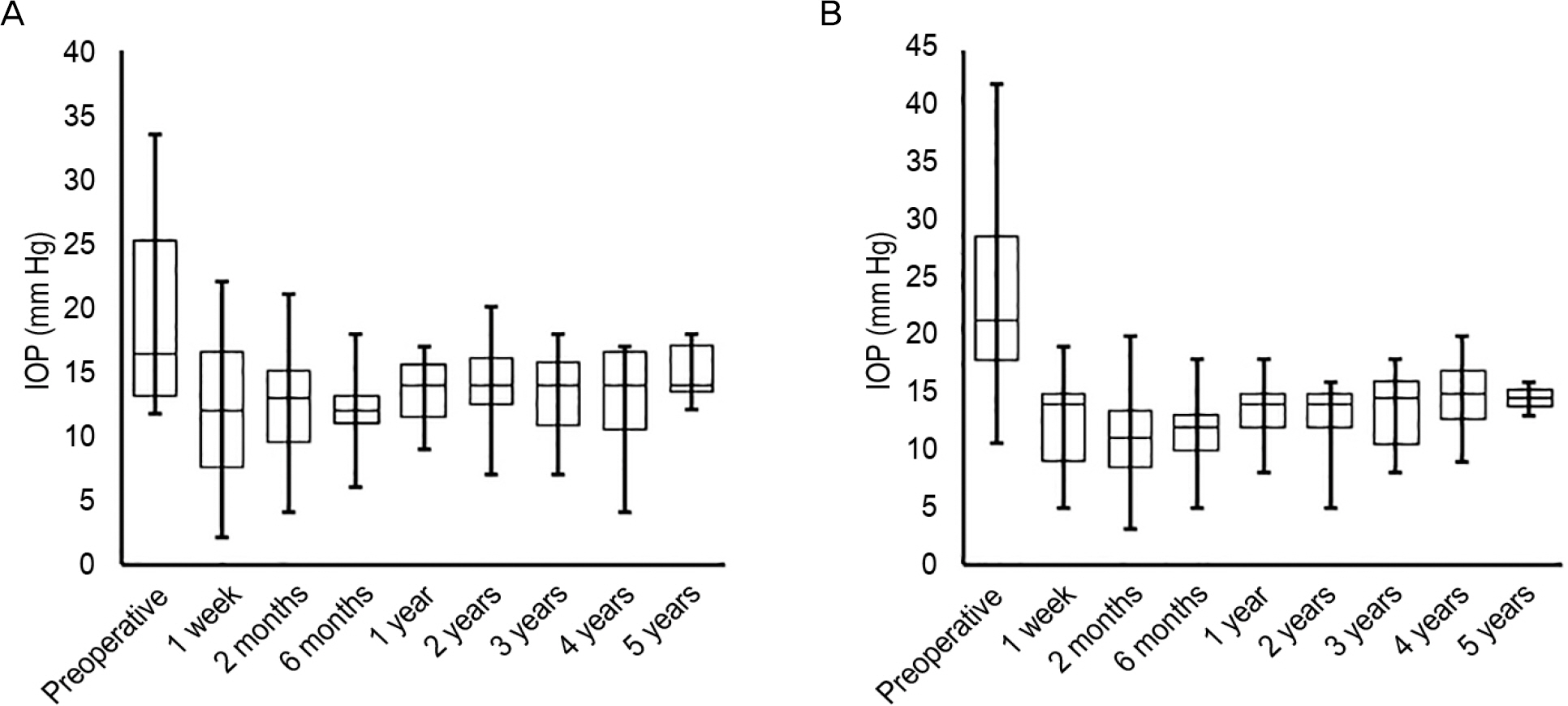
The patients who underwent triple procedures for open-angle glaucoma and angle-closure glaucoma and were followed up for more than 1 year postoperatively were retrospectively reviewed. Preoperative and postoperative visual acuity, intraocular pressure (IOP), visual field mean deviation, refractive error, number of medications, and complications were analyzed. The effect of surgery on IOP reduction and refractive error correction was compared.
RESULTS
The IOP at 1 year postoperatively was 13.39 +/- 2.25 mm Hg, 13.41 +/- 2.79 mm Hg (p = 0.981) and IOP reduction was 4.51 +/- 6.35 mm Hg, 9.11 +/- 8.27 mm Hg (p = 0.042) in the open angle glaucoma group and angle closure glaucoma group, respectively. No patient in either group required reoperation due to uncontrolled IOP. The percentage of patients showing postoperative IOP reduction of at least 10% and 20% from baseline IOP was statistically higher in the angle-closure glaucoma group than in the open-angle glaucoma group. Prediction errors were -0.84 +/- 0.88 D and -0.13 +/- 0.65 D in the open-angle glaucoma group and angle-closure glaucoma group, respectively.
CONCLUSIONS
Triple procedure was effective in reducing IOP in both open-angle glaucoma and angle-closure glaucoma patients. The patients with angle-closure glaucoma showed better results in IOP control and refractive error correction compared with patients with angle-closure glaucoma.
MeSH Terms
Figure
Reference
-
References
1. Acton J, Salmon JF, Scholtz R. Extracapsular cataract extraction with posterior chamber lens implantation in primary angle-closure glaucoma. J Cataract Refract Surg. 1997; 23:930–4.
Article2. Ming Zhi Z, Lim AS, Yin Wong T. A pilot study of lens extraction in the management of acute primary angle-closure glaucoma. Am J Ophthalmol. 2003; 135:534–6.
Article3. Strenk SA, Strenk LM, Guo S. Magnetic resonance imaging of the anteroposterior position and thickness of the aging, accommodat-ing, phakic, and pseudophakic ciliary muscle. J Cataract Refract Surg. 2010; 36:235–41.
Article4. Kook MS, Kim HB, Lee SU. Short-term effect of mitomycin-C augmented trabeculectomy on axial length and corneal astigmatism. J Cataract Refract Surg. 2001; 27:518–23.
Article5. Tan HY, Wu SC. Refractive error with optimum intraocular lens power calculation after glaucoma filtering surgery. J Cataract Refract Surg. 2004; 30:2595–7.
Article6. Lowe RF. Aetiology of the anatomical basis for primary angle-clo-sure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol. 1970; 54:161–9.
Article7. George R, Paul PG, Baskaran M, et al. Ocular biometry in occlud-able angles and angle closure glaucoma: a population based survey. Br J Ophthalmol. 2003; 87:399–402.
Article8. Go GB, Kim DW, Baek NH. Intraocular pressure change following cataract surgery in patient with high intraocular pressure. J Korean Ophthalmol Soc. 1993; 34:1128–34.9. Martinez-Bello C, Rodriguez-Ares T, Pazos B, et al. Changes in anterior chamber depth and angle width after filtration surgery: a quantitative study using ultrasound biomicroscopy. J Glaucoma. 2000; 9:51–5.10. Karasheva G, Goebel W, Klink T, et al. Changes in macular thick-ness and depth of anterior chamber in patients after filtration surgery. Graefes Arch Clin Exp Ophthalmol. 2003; 241:170–5.
Article11. Francis BA, Wang M, Lei H, et al. Changes in axial length follow-ing trabeculectomy and glaucoma drainage device surgery. Br J Ophthalmol. 2005; 89:17–20.
Article12. Uretmen O, Ateş H, Andaç K, Deli B. Axial length changes accom-panying successful nonpenetrating glaucoma filtration surgery. Ophthalmologica. 2003; 217:199–203.
Article13. Chan JC, Lai JS, Tham CC. Comparison of postoperative re-fractive outcome in phacotrabeculectomy and phacoemulsification with posterior chamber intraocular lens implantation. J Glaucoma. 2006; 15:26–9.
Article14. Husain R, Li W, Gazzard G, et al. Longitudinal changes in anterior chamber depth and axial length in Asian subjects after trabeculec-tomy surgery. Br J Ophthalmol. 2013; 97:852–6.
Article15. Caporossi A, Casprini F, Tosi GM, Balestrazzi A. Long-term results of combined 1-way phacoemulsification, intraocular lens im-plantation, and trabeculectomy. J Cataract Refract Surg. 1999; 25:1641–5.
Article16. Rockwood EJ, Larive B, Hahn J. Outcomes of combined cataract extraction, lens implantation, and trabeculectomy surgeries. Am J Ophthalmol. 2000; 130:704–11.
Article17. Tow SL, Aung T, Oen FT, Seah SK. Combined phacoemulsifica-tion, intraocular lens implantation and trabeculectomy for chronic angle closure glaucoma. Int Ophthalmol. 2001; 24:283–9.