Effectiveness of Rehabilitative Balloon Swallowing Treatment on Upper Esophageal Sphincter Relaxation and Pharyngeal Motility for Neurogenic Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Myongji Hospital, Goyang, Korea. jeonggyu.yoon@gmail.com
- KMID: 2148222
- DOI: http://doi.org/10.5535/arm.2015.39.4.524
Abstract
OBJECTIVE
To investigate the relationship between dysphagia severity and opening of the upper esophageal sphincter (UES), and to assess the effect of balloon size on functional improvement after rehabilitative balloon swallowing treatment in patients with severe dysphagia with cricopharyngeus muscle dysfunction (CPD).
METHODS
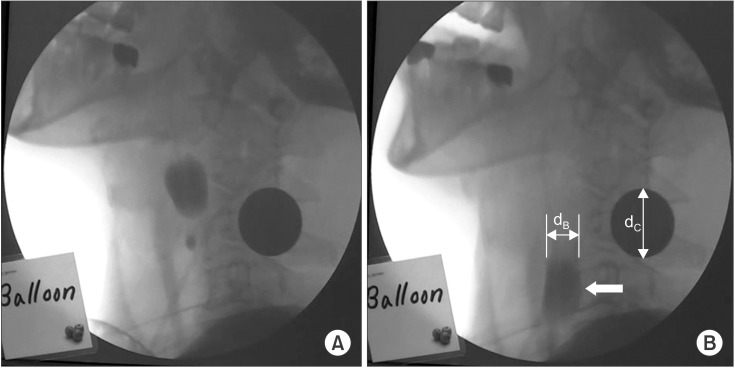
We reviewed videofluoroscopic swallowing studies (VFSS) conducted in the Department of Physical Medicine and Rehabilitation, Myongji Hospital from January through December in 2012. All subjects diagnosed with CPD by VFSS further swallowed a 16-Fr Foley catheter filled with barium sulfate suspension for three to five minutes. We measured the maximum diameter of the balloon that a patient could swallow into the esophagus and subsequently conducted a second VFSS. Then, we applied a statistical technique to correlate the balloon diameter with functional improvement after the balloon treatment.
RESULTS
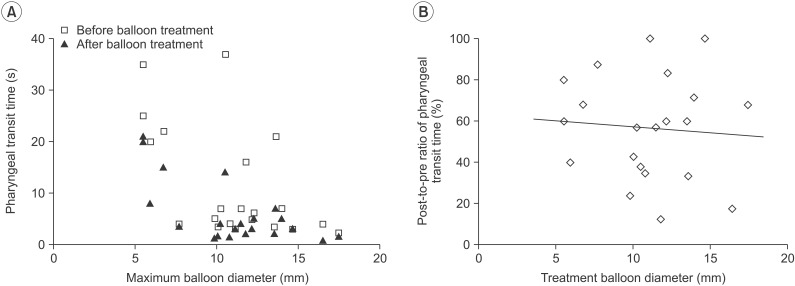
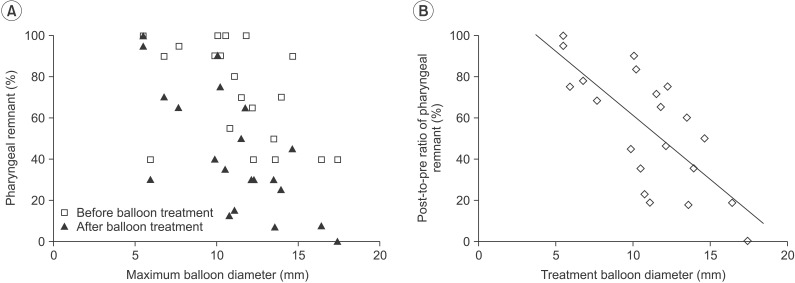
Among 283 inpatients who received VFSS, 21 subjects were diagnosed with CPD. It was observed that the degree of UES opening evaluated by swallowing a catheter balloon had inverse linear correlations with pharyngeal transit time and post-swallow pharyngeal remnant. Videofluoroscopy guided iterative balloon swallowing treatment for three to five minutes, significantly improved the swallowing ability in terms of pharyngeal transit time and pharyngeal remnant (p<0.005 and p<0.001, respectively). Correlation was seen between balloon size and reduction in pharyngeal remnants after balloon treatment (Pearson correlation coefficient R=-0.729, p<0.001), whereas there was no definite relationship between balloon size and improvement in pharyngeal transit time (R=-0.078, p=0.738).
CONCLUSION
The maximum size of the balloon that a patient with CPD can swallow possibly indicates the maximum UES opening. The iterative balloon swallowing treatment is safe without the risk of aspiration, and it can be an effective technique to improve both pharyngeal motility and UES relaxation.
MeSH Terms
Figure
Cited by 4 articles
-
Effect of Vallecular Ballooning in Stroke Patients With Dysphagia
Yong Kyun Kim, Sang-heon Lee, Jang-won Lee
Ann Rehabil Med. 2017;41(2):231-238. doi: 10.5535/arm.2017.41.2.231.Effects of Capping of the Tracheostomy Tube in Stroke Patients With Dysphagia
Yong kyun Kim, Sang-heon Lee, Jang-won Lee
Ann Rehabil Med. 2017;41(3):426-433. doi: 10.5535/arm.2017.41.3.426.Efficacy of a 4-Week Swallowing Rehabilitation Program Combined With Pyriform Sinus Ballooning in Patients With Post-stroke Dysphagia
Yong Kyun Kim, Kyun Yeon Lee, Sang-Heon Lee
Ann Rehabil Med. 2018;42(4):542-550. doi: 10.5535/arm.2018.42.4.542.Comparison of Dysphagia Between Infratentorial and Supratentorial Stroke Patients
Yong Kyun Kim, Jung Hyun Cha, Kyun Yeon Lee
Ann Rehabil Med. 2019;43(2):149-155. doi: 10.5535/arm.2019.43.2.149.
Reference
-
1. Haapaniemi JJ, Laurikainen EA, Pulkkinen J, Marttila RJ. Botulinum toxin in the treatment of cricopharyngeal dysphagia. Dysphagia. 2001; 16:171–175.
Article2. Alfonsi E, Merlo IM, Ponzio M, Montomoli C, Tassorelli C, Biancardi C, et al. An electrophysiological approach to the diagnosis of neurogenic dysphagia: implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatry. 2010; 81:54–60. PMID: 19762326.
Article3. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335.
Article4. Terre R, Mearin F. Oropharyngeal dysphagia after the acute phase of stroke: predictors of aspiration. Neurogastroenterol Motil. 2006; 18:200–205.
Article5. Jones CA, Hammer MJ, Hoffman MR, McCulloch TM. Quantifying contributions of the cricopharyngeus to upper esophageal sphincter pressure changes by means of intramuscular electromyography and high-resolution manometry. Ann Otol Rhinol Laryngol. 2014; 123:174–182. PMID: 24633943.
Article6. Ertekin C, Aydogdu I. Electromyography of human cricopharyngeal muscle of the upper esophageal sphincter. Muscle Nerve. 2002; 26:729–739.
Article7. Kuhn MA, Belafsky PC. Management of cricopharyngeus muscle dysfunction. Otolaryngol Clin North Am. 2013; 46:1087–1099.
Article8. Solt J, Bajor J, Moizs M, Grexa E, Horvath PO. Primary cricopharyngeal dysfunction: treatment with balloon catheter dilatation. Gastrointest Endosc. 2001; 54:767–771. PMID: 11726859.
Article9. Schneider I, Thumfart WF, Pototschnig C, Eckel HE. Treatment of dysfunction of the cricopharyngeal muscle with botulinum A toxin: introduction of a new, noninvasive method. Ann Otol Rhinol Laryngol. 1994; 01; 103:31–35. PMID: 8291857.
Article10. Kelly JH. Management of upper esophageal sphincter disorders: indications and complications of myotomy. Am J Med. 2000; 108(Suppl 4a):43S–46S. PMID: 10718451.
Article11. Dou Z, Zu Y, Wen H, Wan G, Jiang L, Hu Y. The effect of different catheter balloon dilatation modes on cricopharyngeal dysfunction in patients with dysphagia. Dysphagia. 2012; 27:514–520. PMID: 22427310.
Article12. Madanick RD, Shaheen NJ, Dellon ES. A novel balloon pull-through technique for esophageal dilation in eosinophilic esophagitis (with video). Gastrointest Endosc. 2011; 73:138–142. PMID: 21184880.
Article13. Kim JC, Kim JS, Jung JH, Kim YK. The effect of balloon dilatation through video-fluoroscopic swallowing study (VFSS) in stroke patients with cricopharyngeal dysfunction. J Korean Acad Rehabil Med. 2011; 35:23–26.14. Jung B, Choi I, Lee NJ, Jung KI, Yoo WK, Ohn SH. Videofluoroscopy-guided balloon dilatation for the opening dysfunction of upper esophageal sphincter by postoperative vagus nerve injury: a report on two cases. Ann Rehabil Med. 2014; 38:122–126. PMID: 24639936.
Article15. Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005; 86:1516–1520. PMID: 16084801.
Article16. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article17. Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, et al. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002; 122:1314–1321. PMID: 11984518.
Article18. Omari TI, Ferris L, Dejaeger E, Tack J, Vanbeckevoort D, Rommel N. Upper esophageal sphincter impedance as a marker of sphincter opening diameter. Am J Physiol Gastrointest Liver Physiol. 2012; 302:G909–G913. PMID: 22323128.
Article19. Lin T, Xu G, Dou Z, Lan Y, Yu F, Jiang L. Effect of bolus volume on pharyngeal swallowing assessed by high-resolution manometry. Physiol Behav. 2014; 128:46–51. PMID: 24518872.
Article20. Belafsky PC, Plowman EK, Mehdizadeh O, Cates D, Domer A, Yen K. The upper esophageal sphincter is not round: a pilot study evaluating a novel, physiology-based approach to upper esophageal sphincter dilation. Ann Otol Rhinol Laryngol. 2013; 122:217–221. PMID: 23697317.
Article21. Rees CJ, Fordham T, Belafsky PC. Transnasal balloon dilation of the esophagus. Arch Otolaryngol Head Neck Surg. 2009; 135:781–783. PMID: 19687398.
Article22. You DS, Chun MH, Kim HJ, Ryu JS, Song YJ, Park EJ, et al. The effectiveness of oro-esophageal tube feeding with dysphagia after brainstem stroke. J Korean Acad Rehabil Med. 2011; 35:27–33.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to Perform and Interpret Upper Esophageal Sphincter Manometry
- Diagnosis With Manometry and Treatment With Repetitive Transcranial Magnetic Stimulation in Dysphagia
- Physiology of Upper Esophageal Sphincter Contraction
- Effectiveness of the Self-Balloon Dilatation Treatment Dysphagia in Lateral Medullary Infarction: A Case Report
- The Effect of Balloon Dilatation through Video-Fluoroscopic Swallowing Study (VFSS) in Stroke Patients with Cricopharyngeal Dysfunction