Korean Circ J.
2013 Jul;43(7):474-480. 10.4070/kcj.2013.43.7.474.
Inadvertently Developed Ventricular Fibrillation during Electrophysiologic Study and Catheter Ablation: Incidence, Cause, and Prognosis
- Affiliations
-
- 1Division of Cardiology, Korea University College of Medicine, Seoul, Korea. yhkmd@unitel.co.kr
- 2Division of Cardiology, Department of Internal Medicine, Gachon University, Incheon, Korea.
- KMID: 2145503
- DOI: http://doi.org/10.4070/kcj.2013.43.7.474
Abstract
- BACKGROUND AND OBJECTIVES
Ventricular fibrillation (VF) can inadvertently occur during electrophysiologic study (EPS) or catheter ablation. We investigated the incidence, cause, and progress of inadvertently developed VF during EPS and catheter ablation.
SUBJECTS AND METHODS
We reviewed patients who had developed inadvertent VF during EPS or catheter ablation. Patients who developed VF during programmed ventricular stimulation to induce ventricular tachycardia or VF were excluded.
RESULTS
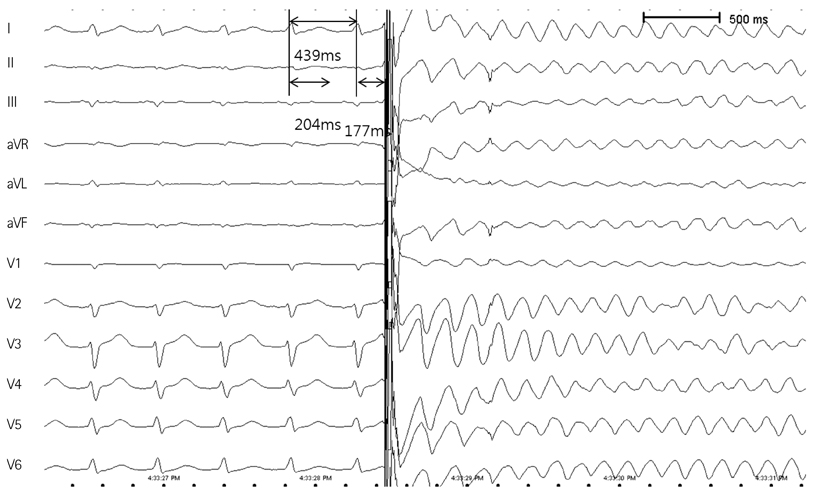
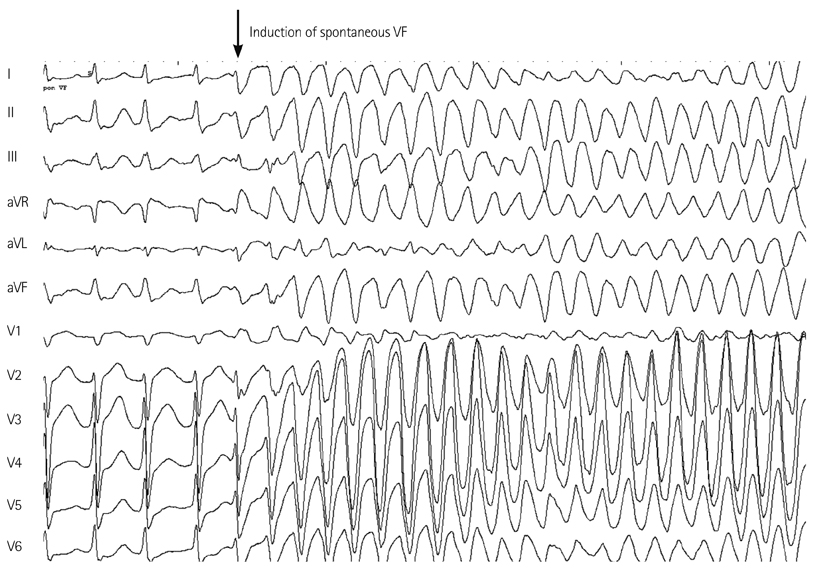
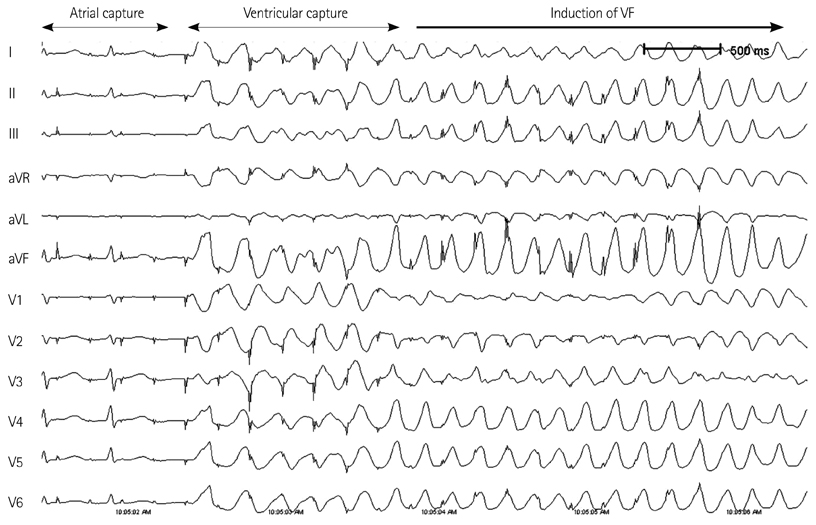
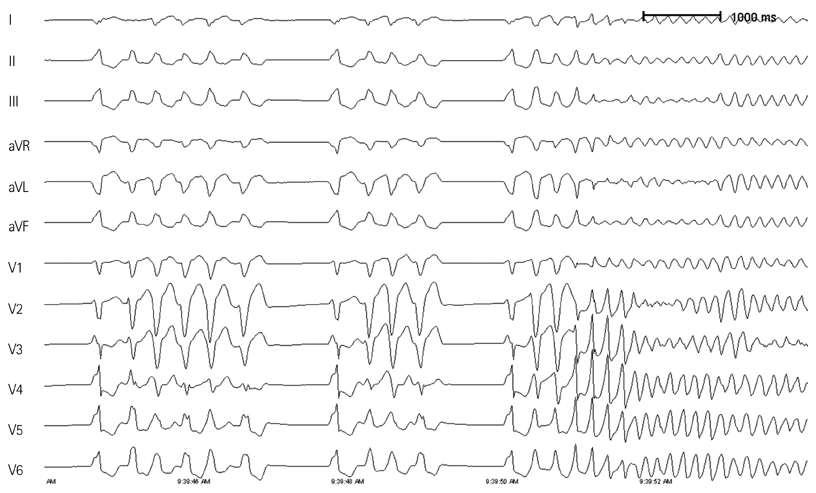
Inadvertent VF developed in 11 patients (46.7+/-9.3 years old) among 2624 patients (0.42%); during catheter ablation for atrial fibrillation (AF) in nine patients, frequent ventricular premature beats (VPBs) in one, and Wolff-Parkinson-White (WPW) syndrome were observed in one. VF was induced after internal cardioversion in six AF patients due to incorrect R-wave synchronization of a direct current shock. Two AF patients showed spontaneous VF induction during isoproterenol infusion while looking for AF triggering foci. The remaining AF patient developed VF after rapid atrial pacing to induce AF, but the catheter was accidentally moved to the right ventricular (RV) apex. A patient with VPB ablation spontaneously developed VF during isoproterenol infusion. The focus of VPB was in the RV outflow tract and successfully ablated. A patient with WPW syndrome developed VF after rapid RV pacing with a cycle length of 240 ms. Single high energy (biphasic 150-200 J) external defibrillation was successful in all patients, except in two, who spontaneously terminated VF. The procedure was uneventfully completed in all patients. At a mean follow-up period of 17.4+/-15.5 months, no patient presented with ventricular arrhythmia.
CONCLUSION
Although rare, inadvertent VF can develop during EPS or catheter ablation. Special caution is required to avoid incidental VF during internal cardioversion, especially under isoproterenol infusion.
MeSH Terms
Figure
Reference
-
1. Denes P, Ezri MD. Clinical electrophysiology--a decade of progress. J Am Coll Cardiol. 1983; 1:292–305.2. Scheinman MM, Morady F. Invasive cardiac electrophysiologic testing: the current state of the art. Circulation. 1983; 67:1169–1173.3. Surawicz B. Intracardiac extrastimulation studies: How to? Where? By whom? Circulation. 1982; 65:428–431.4. Kanda M, Shimizu W, Matsuo K, et al. Electrophysiologic characteristics and implications of induced ventricular fibrillation in symptomatic patients with Brugada syndrome. J Am Coll Cardiol. 2002; 39:1799–1805.5. Horowitz LN, Kay HR, Kutalek SP, et al. Risks and complications of clinical cardiac electrophysiologic studies: a prospective analysis of 1,000 consecutive patients. J Am Coll Cardiol. 1987; 9:1261–1268.6. Murgatroyd FD, Slade AK, Sopher SM, Rowland E, Ward DE, Camm AJ. Efficacy and tolerability of transvenous low energy cardioversion of paroxysmal atrial fibrillation in humans. J Am Coll Cardiol. 1995; 25:1347–1353.7. Cooper RA, Alferness CA, Smith WM, Ideker RE. Internal cardioversion of atrial fibrillation in sheep. Circulation. 1993; 87:1673–1686.8. Kettering K, Mewis C, Riemer M, Kühlkamp V. [Ventricular fibrillation in intra-atrial cardioversion of atrial fibrillation]. Z Kardiol. 2000; 89:269–273.9. Barold HS, Wharton JM. Ventricular fibrillation resulting from synchronized internal atrial defibrillation in a patient with ventricular preexcitation. J Cardiovasc Electrophysiol. 1997; 8:436–440.10. Sharma AD, Waxman MB, Huerta FI. Effect of adrenergic stimulation and blockade on ventricular defibrillation in the rat. J Pharmacol Exp Ther. 1983; 227:716–722.11. Opie LH, Nathan D, Lubbe WF. Biochemical aspects of arrhythmogenesis and ventricular fibrillation. Am J Cardiol. 1979; 43:131–148.12. Rosenthal RE, Turbiak TW. Open-chest cardiopulmonary resuscitation. Am J Emerg Med. 1986; 4:248–258.13. Cohen TJ, Scheinman MM, Pullen BT, et al. Emergency intracardiac defibrillation for refractory ventricular fibrillation during routine electrophysiologic study. J Am Coll Cardiol. 1991; 18:1280–1284.14. Babbs CF, Paris RL, Tacker WA Jr, Bourland JD. Effects of myocardial infarction on catheter defibrillation threshold. Med Instrum. 1983; 17:18–20.15. Marinchak RA, Friehling TD, Kline RA, Stohler J, Kowey PR. Effect of antiarrhythmic drugs on defibrillation threshold: case report of an adverse effect of mexiletine and review of the literature. Pacing Clin Electrophysiol. 1988; 11:7–12.16. Guarnieri T, Levine JH, Veltri EP, et al. Success of chronic defibrillation and the role of antiarrhythmic drugs with the automatic implantable cardioverter/defibrillator. Am J Cardiol. 1987; 60:1061–1064.17. Lerman BB, Halperin HR, Tsitlik JE, Brin K, Clark CW, Deale OC. Relationship between canine transthoracic impedance and defibrillation threshold. Evidence for current-based defibrillation. J Clin Invest. 1987; 80:797–803.18. Winkle RA, Mead RH, Ruder MA, Smith NA, Buch WS, Gaudiani VA. Effect of duration of ventricular fibrillation on defibrillation efficacy in humans. Circulation. 1990; 81:1477–1481.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Successful Ablation of Right-Sided Accessory Pathway during Atrial Fibrillation
- Large Circular Ring Catheter Ablation Versus Anatomically Guided Ablation of Atrial Fibrillation: Back to the Future for Successful Catheter Ablation of Atrial Fibrillation?
- Catheter ablation for treatment of tachyarrhythmia
- A Case of Chronic Radiodermatitis following Radiofrequency Catheter Ablation for Atrial Fibrillation
- Electrical Storm Late after Surgery for a Double-Chambered Right Ventricle, Aortic Regurgitation and a Ventricular Septal Defect: A Case of Successful Catheter Ablation