Korean Circ J.
2014 May;44(3):156-161. 10.4070/kcj.2014.44.3.156.
A Pilot Study of Target Weight Guided Treatment in Acute Heart Failure Using Ultrafiltration or Usual Care: Effect on Sodium Removal
- Affiliations
-
- 1The Christ Hospital Heart and Vascular Center, Cincinnati, OH, USA. chunge@ohioheart.org
- KMID: 2145476
- DOI: http://doi.org/10.4070/kcj.2014.44.3.156
Abstract
- BACKGROUND AND OBJECTIVES
In the Ultrafiltration versus Intravenous Diuretics for Patients Hospitalized for Acute Decompensated Heart Failure trial, ultrafiltration (UF) removed volume more effectively than usual care (UC). Hypothetically, UF may be superior to UC due to increased sodium (Na) removal and less neurohormonal activation. We compared UF and UC in a randomized pilot trial of target weight guided therapy for acute decompensated heart failure (ADHF).
SUBJECTS AND METHODS
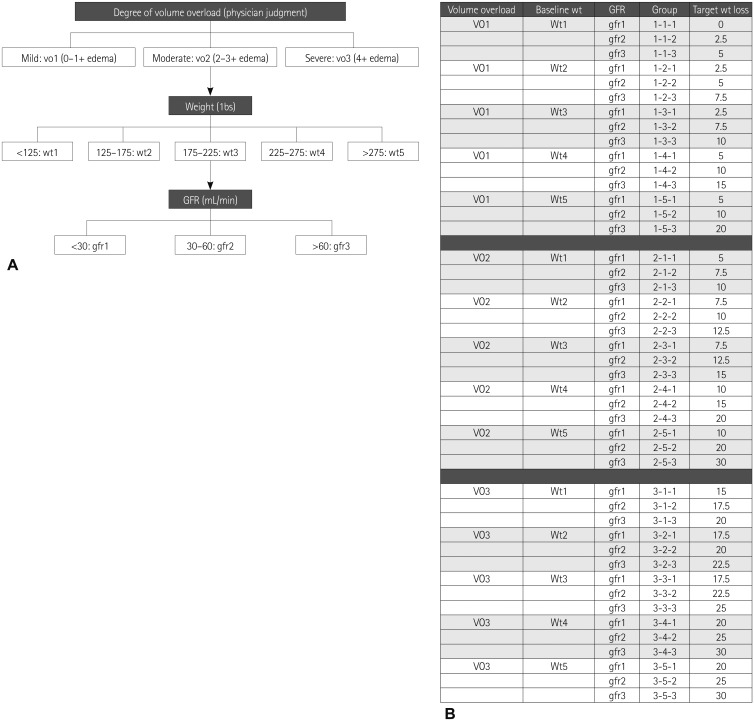
Sixteen patients with ADHF were enrolled and target weights established prospectively, prior to randomization to UC or UF. UF patients did not receive diuretics and UC patients were all treated with a continuous furosemide drip. All urine and ultrafiltrate were collected and Na concentrations measured.
RESULTS
Similar volumes were removed in UC and UF groups (110105 mL and 107415 mL, respectively) and the UF group also produced 45325 mL of urine. Na concentration was 138+/-6 meq/L in the ultrafiltrate, 85+/-73 meq/L in the UC group's urine, and 26+/-23 meq/L in the UF group's urine. Given the relevant associated volumes, total meq of the Na removed was similar (1168 in UC vs. 1216 in UF). The UF group produced isotonic ultrafiltrate and a higher volume of dilute urine than anticipated.
CONCLUSION
In a randomized pilot study of target weight guided therapy with UC or UF for ADHF, there were no differences in total volumes or Na removed, and lengths of hospital stays were similar. Isotonic fluid loss by UF was accompanied by the production of very dilute urine.
Keyword
MeSH Terms
Figure
Reference
-
1. Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: current state and framework for future research. Circulation. 2005; 112:3958–3968. PMID: 16365214.2. Nieminen MS, Böhm M, Cowie MR, et al. Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J. 2005; 26:384–416. PMID: 15681577.3. Nohria A, Lewis E, Stevenson LW. Medical management of advanced heart failure. JAMA. 2002; 287:628–640. PMID: 11829703.4. Adams KF Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005; 149:209–216. PMID: 15846257.5. Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007; 297:61–70. PMID: 17200476.6. McCurley JM, Hanlon SU, Wei SK, Wedam EF, Michalski M, Haigney MC. Furosemide and the progression of left ventricular dysfunction in experimental heart failure. J Am Coll Cardiol. 2004; 44:1301–1307. PMID: 15364336.7. Neuberg GW, Miller AB, O'Connor CM, et al. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J. 2002; 144:31–38. PMID: 12094185.8. Fauchald P, Forfang K, Amlie J. An evaluation of ultrafiltration as treatment of therapy-resistant cardiac edema. Acta Med Scand. 1986; 219:47–52. PMID: 3953316.9. Rimondini A, Cipolla CM, Della Bella P, et al. Hemofiltration as short-term treatment for refractory congestive heart failure. Am J Med. 1987; 83:43–48. PMID: 3605181.10. Costanzo MR, Saltzberg M, O'Sullivan J, Sobotka P. Early ultrafiltration in patients with decompensated heart failure and diuretic resistance. J Am Coll Cardiol. 2005; 46:2047–2051. PMID: 16325040.11. Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007; 49:675–683. PMID: 17291932.12. Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009; 119:e391–e479. PMID: 19324966.13. Schrier RW. Role of diminished renal function in cardiovascular mortality: marker or pathogenetic factor? J Am Coll Cardiol. 2006; 47:1–8. PMID: 16386657.14. Agostoni P, Marenzi G, Lauri G, et al. Sustained improvement in functional capacity after removal of body fluid with isolated ultrafiltration in chronic cardiac insufficiency: failure of furosemide to provide the same result. Am J Med. 1994; 96:191–199. PMID: 8154506.15. O'Brien TM, Menon S, Stephens T, Mazur W, Chung ES. Algorithm-based assessment of target weight removal in acute decompensated heart failure. Congest Heart Fail. 2012; 18:43–46. PMID: 22277177.16. Rogers HL, Marshall J, Bock J, et al. A randomized, controlled trial of the renal effects of ultrafiltration as compared to furosemide in patients with acute decompensated heart failure. J Card Fail. 2008; 14:1–5. PMID: 18226766.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of overnight D/P sodium test in continuous ambulatory peritoneal dialysis
- Low volume peritoneal dialysis in newborns and infants
- Pathophysiology of Cardiorenal Syndrome and Use of Diuretics and Ultrafiltration as Volume Control
- The Effect of Gradient Ultrafiltration and High Sodium Dialysate on Reducing Complications During Hemodialysis
- Medical Treatment of Acute Decompensated Heart Failure Syndrome