Korean J Urol.
2006 Dec;47(12):1334-1338. 10.4111/kju.2006.47.12.1334.
The Long Term Effect of Extracorporeal Magnetic Innervation Therapy with Pelvic Floor Muscle Exercise for Stress Urinary Incontinence
- Affiliations
-
- 1Department of Urology, College of Medicine, Ewha Womans University, Seoul, Korea. bonstone@ewha.ac.kr
- KMID: 2139780
- DOI: http://doi.org/10.4111/kju.2006.47.12.1334
Abstract
- PURPOSE
Extracorporeal magnetic innervation (ExMI) therapy has been known to be safe and immediately effective in stress urinary incontinence (SUI). However, no long term follow-up results have been reported. Therefore; herein, are reported our results from a two year follow-up study on ExMI therapy, with pelvic floor muscle exercises, for SUI.
MATERIALS AND METHODS
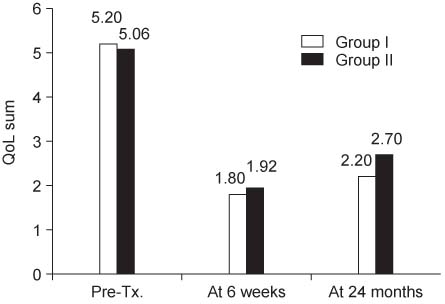
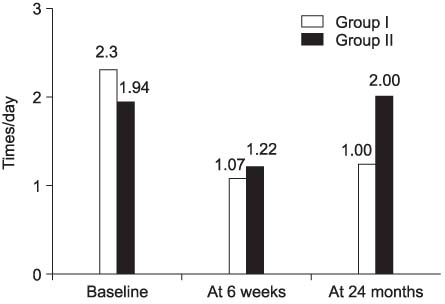
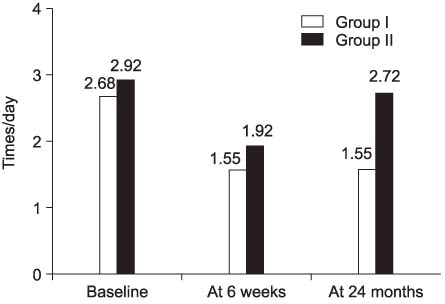
The study group was comprised of 94 patients with SUI. ExMI therapy was performed for 20 minutes (10Hz and 50Hz for each 10 minutes), twice a week, for 6 weeks. Thereafter, 44 of the 94 patients underwent pelvic floor muscle exercises. Objective measures (quality-of-life surveys, pad changes, and leak episodes per day) were evaluated before, immediately after and 24 months after the ExMI therapy.
RESULTS
After 6-week of ExMI therapy, the quality-of-life score improved from 5.1+/-0.9 to 1.8+/-1.1. The mean frequency of pad changes was reduced from 2.1+/-1.6 to 1.1+/-1.0. The mean frequency of leak episodes was also reduced from 2.8+/-1.8 to 1.7+/-1.5 times. After 24 months, the 44 patients having also undergone pelvic floor muscle exercise had persistent improvements in their leak episodes per day compared to the 50 patients that had not.
CONCLUSIONS
When ExMI therapy was followed by pelvic floor muscle exercises, the favorable effect in leak episodes per day after ExMI therapy may persist for at least 24 months.
Keyword
Figure
Reference
-
1. Choo MS. Trends in the surgical treatment of female stress urinary incontinence. Korean J Urol. 2004. 45:509–517.2. Bourcier AP, Juras JC. Nonsurgical therapy for stress incontinence. Urol Clin North Am. 1995. 22:613–627.3. Kegel AH. Progressive resistance exercise in the functional restoration of the perineal muscle. Am J Obstet Gynecol. 1948. 56:238–249.4. Knight S, Laycock J. The role of biofeedback in pelvic floor re-education. Physiotherapy. 1994. 86:145–148.5. Luber KM, Wolde-Tsadik G. Efficacy of functional electrical stimulation in treating genuine stress incontinence: a randomized clinical trial. Neurourol Urodyn. 1997. 16:543–551.6. Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlin SJ. Update on extracorporeal magnetic innervation (ExMI) therapy for stress urinary incontinence. Urology. 2000. 56:6 Suppl 1. 82–86.7. Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol female lower urinary tract symptoms questionnaire: development and psychometric testing. Br J Urol. 1996. 77:805–812.8. Donovan JL, Abrams P, Peters TJ, Kay HE, Reynard J, Chapple C, et al. The ICS-'BPH' Study: the psychometric validity and reliability of the ICSmale questionnaire. Br J Urol. 1996. 77:554–562.9. Burgio KL, Mattews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged woman. J Urol. 1991. 146:1255–1259.10. Rohner TJ Jr, Rohner JF. O'Donell PD, editor. Further commentary: the social significance. Urinary incontinence. 1997. St. Louis: Mosby-Year Book;4–6.11. Ueda T, Tamaki M, Kageyama S, Yoshimura N, Yoshida D. Urinary incontinence among community-dwelling people aged 40 years or older in Japan: prevalence, risk factors, knowledge and self-perception. Int J Urol. 2000. 7:95–103.12. Kim UH, Kim YH, Kim ME. The prevalence and quality of life of overactive bladder and urinary incontinence in young women. Korean J Urol. 2004. 45:543–550.13. Seo JB, Lee JZ. The epidemiologic study of the urinary incontinence in community-dwelling women over 50 years old. Korean J Urol. 1999. 40:1525–1530.14. Kim JS, Lee JZ. The prevalence of urinary incontinence in elderly women at institutionalized facilities in pusan. Korean J Urol. 1999. 40:1019–1023.15. Yamanishi T, Yasuda K, Sakakibara R, Hattori T, Ito H, Murakami S. Pelvic floor electrical stimulation in the treatment of stress incontinence: an investigational study and a placebocontrolled double-blind trial. J Urol. 1997. 158:2127–2131.16. Barker AT, Freeston IL, Jalinous R, Jarratt JA. Magnetic stimulation of the human brain and peripheral nervous system: an introduction and the results of an initial clinical evaluation. Neurosurgery. 1987. 20:100–109.17. Yamanishi T, Yasuda K, Suda S, Ishikawa N. Effect of functional continuous magnetic stimulation on urethral closure in healthy volunteers. Urology. 1999. 54:652–655.18. Evans BA, Daube JR, Litchy WJ. A comparison of magnetic and electrical stimulation of spinal nerves. Muscle Nerve. 1990. 13:414–420.19. Olney RK, So YT, Goodin DS, Aminoff MJ. A comparison of magnetic and electrical stimulation of peripheral nerves. Muscle Nerve. 1990. 13:957–963.20. Galloway NT, Risk E, El-Galley S, Sand PK, Appell RA, Russell HW, et al. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999. 53:1108–1111.21. Salvatore JR, Weitberg AB, Mehta S. Nonionizing electromagnetic fields and cancer: a review. Oncology. 1996. 10:563–570.22. Yokoyama T, Fujita O, Nishiguchi J, Nozaki K, Nose H, Inoue M, et al. Extracorporeal magnetic innervation treatment for urinary incontinence. Int J Urol. 2004. 11:602–606.23. Kim KH, Hong JY, Yoon H. Early experience with extracorporeal magnetic innervation (ExMI) therapy for stress urinary incontinence. Korean J Urol. 2001. 42:938–941.24. Choi JH, Min KS, Choi SH. Effect of extracorporeal magnetic innervation therapy in patient with stress urinary incontinence. Korean J Urol. 2003. 44:317–321.25. Largo-Janssen T, Van WC. Long term effect of treatment of female incontinence in general practice. Br J Gen Pract. 1998. 48:1735–1738.26. Hahn I, Milson I, Fall M, Ekelund P. Long-term results of pelvic training in female stress urinary incontinence. Br J Urol. 1993. 72:421–427.27. Cammu H, Van Nylen M, Amy JJ. A 10-year follow-up after Kegel pelvic floor muscle exercises for genuine stress incontinence. BJU Int. 2000. 85:655–658.28. Bo K, Talseth T. Long-term effect of pelvic floor muscle exercises 5 years after cessation of organized training. Obstet Gynecol. 1996. 87:261–265.29. Bo K. Effect of electrical stimulation on stress and urge urinary incontinence. Clinical outcome and practical recommendations based on randomized controlled trials. Acta Obstet Gynecol scand. 1998. 168:Suppl. 3–11.30. Fall M. Advantages and pitfalls of functional electrical stimulation. Acta Obstet Gynecol Scand. 1998. 168:Suppl. 16–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Experience with Extracorporeal Magnetic Innervation (ExMI) Therapy for Stress Urinary Incontinence
- The Efficacy of Pelvic Floor Muscle Exercise in Patients with Genuine Stress Incontinence
- The Effects of Pelvic Floor Muscle Exercise on Urinary Symptoms and Quality of Life in Women with Stress Urinary Incontinence
- FES-biofeedback versus intensive pelvic floor muscle exercise for the prevention and treatment of genuine stress incontinence
- Assessment of Pelvic Floor Muscle Exercise using Vaginal Cone in Stress Urinary Incontinence of Korea Women