J Korean Med Assoc.
2006 Jun;49(6):542-552. 10.5124/jkma.2006.49.6.542.
Endovascular Aneurysm Repair
- Affiliations
-
- 1Department of Surgery, Inha University College of Medicine & Hospital, Korea. keechong@inha.ac.kr
- 2Department of Radiology, Inha University College of Medicine & Hospital, Korea.
- KMID: 2137834
- DOI: http://doi.org/10.5124/jkma.2006.49.6.542
Abstract
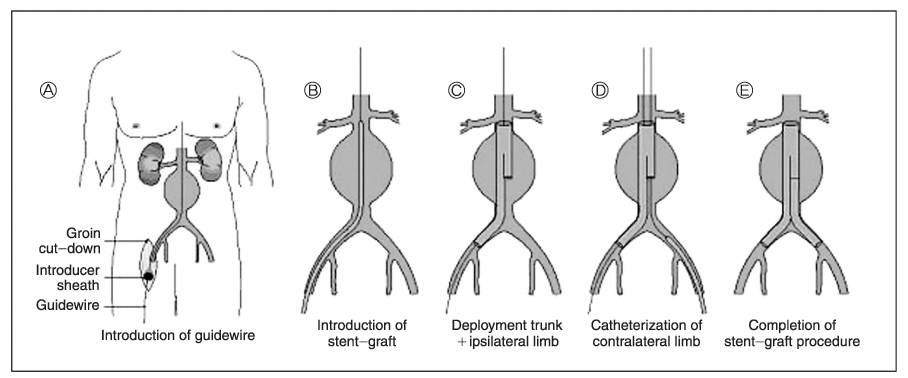
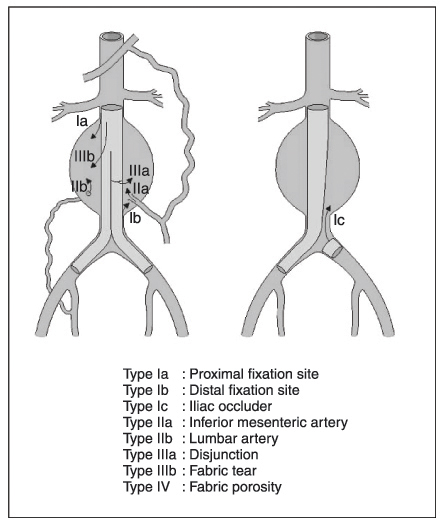
- In recent years, the interest in minimally invasive surgery has grown, and the same trend is observed in vascular surgery and interventional radiology, leading to what is called endovascular surgery. Since the first use of a stent-graft for the endovascular exclusion of an abdominal aortic aneurysm (AAA), endovascular aneurysm repair (EVAR) has greatly expanded, and more than 50,000 devices have been implanted until now. The endovascular graft can be implanted from a remote access site in the groin with a less anesthetic requirement. The endovascular graft is advanced over guidewires up the femoral and iliac arteries. Once in position, the graft is deployed immediately distal from the renal arteries. The aorta is not clamped and the blood loss is less than with open surgery. EVAR for AAA offers an important new alternative to open surgical procedure. The mortality rates after EVAR are reported between 0~5%. Long-term follow-up reports are not available, but mid-term follow-up of EVAR reveals an incidence of re-intervention between 10~20% and a rate of late rupture of between 0.5~1.5% per year. The problems of endoleaks and graft failure continue to be the challenges that require technological innovations. Based on the currently available evidence, EVAR is an appropriate treatment for selected patients, especially those at high risk for open surgical repair.
Keyword
MeSH Terms
Figure
Reference
-
1. Dos Santos JC. Sur La des obstruction des thrombose arterielle anciennes. Med Acad Chir. 1947. 409–411.2. Vollmar J. Rekonstruktive chirurgie der arterien. 1967. Stuttgart: 24–27. 264–270.3. Sternburgh WC III, Carter G, York JW. Aortic neck angulation predicts adverse outcome with endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2002. 35:482–486.
Article4. Stanely BM, Semmens JB, Mai Q. Evaluation of patient selection guidelines for endoluminal AAA repair with the Zenith stent-graft: the Australian experience. J Endovasc Ther. 2001. 8:457–464.
Article5. Beebe HG. Imaging modalities for aortic endografting. J Endovasc Surg. 1997. 4:111–123.
Article6. Broeders IAMJ, Blankensteijn JD. A simple technique to improve the accuracy of proximal AAA endograft deployment. J Endovasc Ther. 2000. 7:389–393.
Article7. May J, White GH. Rutherford R, editor. Endovascular treatment of aortic aneurysm. Vascular surgery. 1999. 5th ed. Philadelphia: WB Saunders;1281–1295.8. Brewster DC, Geller CS, Kaufmann JA. Initial experience with endovascular aneurysm repair: comparison of early results with outcome of conventional open repair. J vasc Surg. 1998. 27:992–1003.9. De Virgilio C, Bui H, Donayre C. Endovascularvs open abdominal aortic aneurysm repair. Arch Surg. 1999. 134:947–951.
Article10. Beebe HG, Cronewett JL, Katzen BT. Results of an aortic endograft trial: impact of device failure beyond 12 months. J Vasc Surg. 2001. 33:S55–S63.
Article11. White GH, Yu W, May J. Endoleaks as a complication of endoluminal grafting of abdominal aortic aneurysm: classification, incidence, diagnosis and management. J Endovasc Surg. 1997. 4:152–168.
Article12. White GH, May J, Waugh R, et al. Type I and type II endoleak: a more useful classification for reporting results of endoluminal repair of AAA. J Endovasc Surg. 1998. 5:189–191.
Article13. Schrink GW, Aarts N, Wilde J. Endoleakage after stent-graft treatment of abdominal aneurysms: implications on pressure and imaging: an in-vitro study. J Vasc Surg. 1998. 28:234–241.14. Faries PL, Sanchez LA, Martin ML. An experimental model for the acute and chronic evaluation of intra-aneurysmal pressure. J Endovasc Surg. 1997. 4:290–297.
Article15. Moore WS, Rutherford RB. EVT Investigators. Transfemoral endovascular repair of abdominal aortic aneurysm: results of the North American EVT phase 1 trial. J Vasc Surg. 1996. 23:543–553.
Article16. Blum U, Voshage G, Lammer J. Endoluminal stent-grafts for infrarenal abdominal aneurysms. N Engl J Med. 1997. 336:13–20.
Article17. Schlensak C, Doenst T, Moreno JB, et al. Serious complications requiring surgical interventions after endoluminal stent graft placement for the treatment of infrarenal aortic aneurysms. J Vasc Surg. 2001. 34:198–203.
Article18. Sonesson B, Lanne T, Hansen F, Sandgren T. Infrarenal aortic diameter in the healthy person. Eur J Vasc Surg. 1994. 8:89–95.
Article19. Zarins CK, White RA, Moll FL. Aneurysm rupture after endovascular repair using the AneuRx stent graft. J Vasc Surg. 2000. 31:960–970.
Article20. Makaroun MS. The Ancure endografting system: an update. J Vasc Surg. 2001. 33:S129–S134.
Article21. Sato DT, Goff CD, Gregory RT, et al. Endoleak after aortic stent graft repair: diagnosis by color duplex ultrasound versus computed tomography. J Vasc Surg. 1998. 28:657–663.
Article22. Cuypers PW, Laheij RJ, Buth J. Which factors increase the risk of conversion to open surgery following endovascular abdominal aortic aneurysm repair? The EUROSTAR collaborators. Eur J Vasc Endovasc Surg. 2000. 20:183–189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Repair of Thoracic Aortic Aneurysm Using a Custom-made Fenestrated Stent Graft to Preserve the Left Subclavian Artery
- Novel Technique to Rescue a Folded Aortic Endograft during Endovascular Aneurysm Repair
- Endovascular Repair of a Juxtarenal Abdominal Aortic Aneurysm Using a Chimney Graft
- Endovascular Treatment of Abdominal Aortic Aneurysm
- Visceral Debranching Thoracic Endovascular Aneurysm Repair for Chronic Dissecting Thoracoabdominal Aortic Aneurysm