Ewha Med J.
2012 Mar;35(1):49-53. 10.12771/emj.2012.35.1.49.
A Case of Ileal Mesenteric Desmoid Tumor Resected by Laparoscopic Surgery
- Affiliations
-
- 1Department of Surgery, Ewha Womans University School of Medicine, Seoul, Korea. ralee@ewha.ac.kr
- 2Department of Pathology, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2134946
- DOI: http://doi.org/10.12771/emj.2012.35.1.49
Abstract
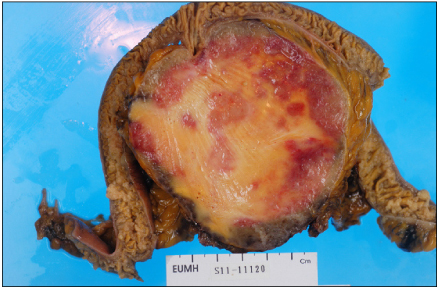
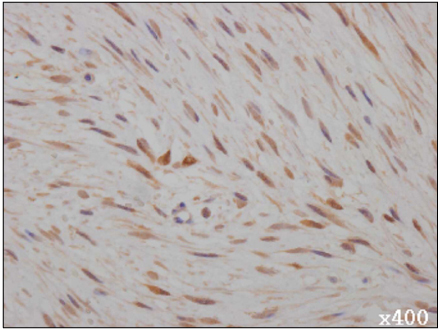
- Desmoid tumor is rare neoplasm originated from fibrous sheath or musculoaponeurotic structure. It is classified as benign tumor histologically, but clinically, it has malignant characteristics due to its infiltrative growth to adjacent organ and frequent local recurrence. Especially, mesenteric desmoid tumor shows poor prognosis because of its symptoms of pain, intestinal obstruction, ureter obstruction and fistula formation and high frequency of recurrence. We experienced a case of mesenteric desmoid tumor in a 64-year-old woman with a painless abdominal mass. Laparoscopic exploration was performed and 10 cm sized mesenteric mass was identified, which resected widely and the diagnosis was confirmed with desmoid tumor by pathologic report. We reviewed the feature of the mesenteric desmoid tumor, that is, pathophysiology, clinical presentations, diagnosis, treatment and prognosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Kulaylat MN, Karakousis CP, Keaney CM, McCorvey D, Bem J, Ambrus JL Sr. Desmoid tumour: a pleomorphic lesion. Eur J Surg Oncol. 1999. 25:487–497.2. Kawashima A, Goldman SM, Fishman EK, Kuhlman JE, Onitsuka H, Fukuya T, et al. CT of intraabdominal desmoid tumors: is the tumor different in patients with Gardner's disease? AJR Am J Roentgenol. 1994. 162:339–342.3. Park BH, Kim HJ, Chang YW, Kim KJ, Lee DK, Dong SH, et al. Desmoid tumor and duodenal adenoma in a patient with familial adenomatous polyposis: a case report. Korean J Gastrointest Endosc. 2001. 23:32–35.4. Lee HS, Jeon HM, Ok ST, Kim JS, Lee EJ, Kim JS. Unresectable desmoid tumor developing after surgery of F.A.P case report. J Korean Soc Coloproctol. 1998. 14:323–329.5. Shiu MH, Weinstein L, Hajdu SI, Brennan MF. Malignant soft-tissue tumors of the anterior abdominal wall. Am J Surg. 1989. 158:446–451.6. Venkat D, Levine E, Wise WE. Abdominal pain and colonic obstruction from an intra-abdominal desmoid tumor. Gastroenterol Hepatol (N Y). 2010. 6:662–665.7. Mecrow IK, Miller V, Lendon M, Doig CM. Mesenteric fibromatosis presenting with ascites in childhood. J Pediatr Gastroenterol Nutr. 1990. 11:118–122.8. Bansal M, Shindelman LE, Geller SA, Gordon RE, Schwarz R. Mesenteric fibromatosis. Mt Sinai J Med. 1983. 50:527–530.9. Lee JC, Thomas JM, Phillips S, Fisher C, Moskovic E. Aggressive fibromatosis: MRI features with pathologic correlation. AJR Am J Roentgenol. 2006. 186:247–254.10. Klein WA, Miller HH, Anderson M, DeCosse JJ. The use of indomethacin, sulindac, and tamoxifen for the treatment of desmoid tumors associated with familial polyposis. Cancer. 1987. 60:2863–2868.11. Murayama T, Imoto S, Ito M, Matsushita K, Matozaki S, Nakagawa T, et al. Mesenteric fibromatosis presenting as fever of unknown origin. Am J Gastroenterol. 1992. 87:1503–1505.12. Yu YH, Son BK, Jun DW, Kim SH, Jo YJ, Park YS, et al. A case of desmoid tumor presenting as intra-abdominal abscess. Korean J Gastroenterol. 2009. 53:315–319.13. Forte MD, Brant WE. Spontaneous isolated mesenteric fibromatosis: report of a case. Dis Colon Rectum. 1988. 31:315–317.14. Koppikar MG, Vaze AM, Patel MS, Phadke PP, Chitale AR, Bapat RD. Mesenteric fibromatosis. J Postgrad Med. 1980. 26:196–198.15. Stout AP, Raffaele L. Tumors of the soft tissues. 1967. Washington, DC: Armed Forces Institute of Pathology.16. Moon HH, Yang SI, Yoon KY, Jang HK, Seo KW, Lee SH, et al. Jejunal mesenteric fibromatosis. J Korean Surg Soc. 2010. 78:320–324.17. Monihan JM, Carr NJ, Sobin LH. CD34 immunoexpression in stromal tumours of the gastrointestinal tract and in mesenteric fibromatoses. Histopathology. 1994. 25:469–473.18. Montgomery E, Torbenson MS, Kaushal M, Fisher C, Abraham SC. Beta-catenin immunohistochemistry separates mesenteric fibromatosis from gastrointestinal stro al tumor and sclerosing mesenteritis. Am J Surg Pathol. 2002. 26:1296–1301.19. Nam KH, Kweon BC, Lee HK, Lee DW, Woo CK, Park JS, et al. A case of mesenteric fibromatosis after appendectomy. Korean J Med. 1998. 54:577–581.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of Partial Resection of Desmoid Tumor and Perforated Small Bowel for Unresectable Desmoid Tumor with Small Bowel Perforation after IPAA for FAP
- Unresectable Desmoid Tumor Developing after Surgery of F.A.P Case report
- Jejunal Mesenteric Fibromatosis
- Development of Desmoid and Mesenteric Fibromas following Total Colectomy for Adenomatous Polyposis Coli in Gardner's syndrome
- Giant Mesenteric Lipoma As an Unusual Cause of Abdominal Pain: A Case Report and a Review of the Literature