Korean J Urol.
2015 Feb;56(2):144-149. 10.4111/kju.2015.56.2.144.
Efficacy of scrotal Doppler ultrasonography with the Valsalva maneuver, standing position, and resting-Valsalva ratio for varicocele diagnosis
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea. drmsk@korea.com
- KMID: 2133279
- DOI: http://doi.org/10.4111/kju.2015.56.2.144
Abstract
- PURPOSE
To determine effectiveness of Valsalva maneuver and standing position on scrotal color Doppler ultrasound (CDU) for the varicocele diagnosis.
MATERIALS AND METHODS
We reviewed the physical examination and CDU finding in 87 patients who visited National Police Hospital from January 2011 to April 2014. Diameters of pampiniform plexus were measured bilaterally during resting and Valsalva maneuver in the supine position and standing position. We calculated the ratio of mean of maximal vein diameter (mMVD) during resting and Valsalva maneuver (resting-Valsalva ratio) and compared in the both position.
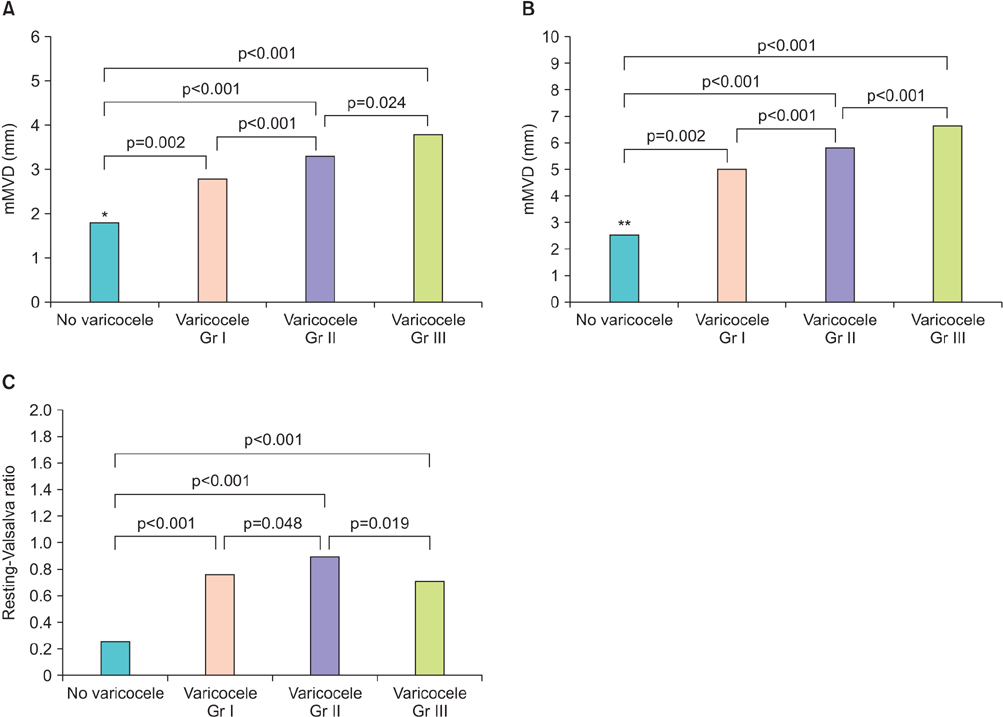
RESULTS
In the resting and supine position, mMVD of varicocele testis units were 1.8 mm, 2.1 mm, 2.6 mm (grades I, II, III, respectively), and that of normal testis units (NTU) 1.2 mm. During Valsalva maneuver in the supine position, mMVD were 3.0 mm, 3.4 mm, 4.2 mm (grades I, II, III) vs 1.8 mm (NTU) (p=0.007, p<0.001, p<0.001, respectively). Average of resting-Valsalva ratio in the supine position were 0.69, 0.74, 0.74 (grades I, II, III) and 0.67 (NTU). Whereas in the resting and standing position, mMVD were 2.8 mm, 3.3 mm, 3.8 mm (grades I, II, III) and 1.8 mm (NTU) (p=0.002, p<0.001, p<0.001). During Valsalva maneuver in the standing position, mMVD were 5.0 mm, 5.8 mm, 6.6 mm (grades I, II, III) and 2.5 mm (NTU) (p=0.002, p<0.001, p<0.001). And average resting-Valsalva ratio were 0.76, 0.90, 0.71 (grades I, II, III) and 0.26 (NTU), which showed significant differences from all grades (p<0.001, p<0.001, p<0.001).
CONCLUSIONS
It is suggested that the standing position and Valsalva maneuver during CDU could improve diagnostic ability for varicocele. Resting-Valsalva ratio in the standing position could be a new diagnostic index for varicocele diagnosis using CDU.
MeSH Terms
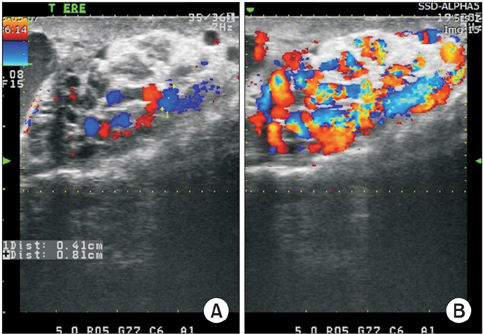
Figure
Reference
-
1. Sigmund G, Gall H, Bahren W. Stop-type and shunt-type varicoceles: venographic findings. Radiology. 1987; 163:105–110.2. Cornud F, Belin X, Amar E, Delafontaine D, Helenon O, Moreau JF. Varicocele: strategies in diagnosis and treatment. Eur Radiol. 1999; 9:536–545.3. Arslan H, Sakarya ME, Atilla MK. Clinical value of power Doppler sonography in the diagnosis of varicocele. J Clin Ultrasound. 1998; 26:229.4. Greenberg SH. Varicocele and male fertility. Fertil Steril. 1977; 28:699–706.5. Cina A, Minnetti M, Pirronti T, Vittoria Spampinato M, Canade A, Oliva G, et al. Sonographic quantitative evaluation of scrotal veins in healthy subjects: normative values and implications for the diagnosis of varicocele. Eur Urol. 2006; 50:345–350.6. Kocakoc E, Serhatlioglu S, Kiris A, Bozgeyik Z, Ozdemir H, Bodakci MN. Color Doppler sonographic evaluation of interrelations between diameter, reflux and flow volume of testicular veins in varicocele. Eur J Radiol. 2003; 47:251–256.7. Kim WS, Choi DY, Han YT. Scrotal Doppler ultrasonography in the assessment of varicocele. Korean J Urol. 1998; 39:1070–1076.8. Wolverson MK, Houttuin E, Heiberg E, Sundaram M, Gregory J. High-resolution real-time sonography of scrotal varicocele. AJR Am J Roentgenol. 1983; 141:775–779.9. Rifkin MD, Foy PM, Kurtz AB, Pasto ME, Goldberg BB. The role of diagnostic ultrasonography in varicocele evaluation. J Ultrasound Med. 1983; 2:271–275.10. Gonda RL Jr, Karo JJ, Forte RA, O'Donnell KT. Diagnosis of subclinical varicocele in infertility. AJR Am J Roentgenol. 1987; 148:71–75.11. Orda R, Sayfan J, Manor H, Witz E, Sofer Y. Diagnosis of varicocele and postoperative evaluation using inguinal ultrasonography. Ann Surg. 1987; 206:99–101.12. Nashan D, Behre HM, Grunert JH, Nieschlag E. Diagnostic value of scrotal sonography in infertile men: report on 658 cases. Andrologia. 1990; 22:387–395.13. Eskew LA, Watson NE, Wolfman N, Bechtold R, Scharling E, Jarow JP. Ultrasonographic diagnosis of varicoceles. Fertil Steril. 1993; 60:693–697.14. Hoekstra T, Witt MA. The correlation of internal spermatic vein palpability with ultrasonographic diameter and reversal of venous flow. J Urol. 1995; 153:82–84.15. Chiou RK, Anderson JC, Wobig RK, Rosinsky DE, Matamoros A Jr, Chen WS, et al. Color Doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. Urology. 1997; 50:953–956.16. Dubin L, Amelar RD. Varicocele size and results of varicocelectomy in selected subfertile men with varicocele. Fertil Steril. 1970; 21:606–609.17. Kim SW. Varicocele and male infertility. J Korean Med Assoc. 2012; 55:37–46.18. Beddy P, Geoghegan T, Browne RF, Torreggiani WC. Testicular varicoceles. Clin Radiol. 2005; 60:1248–1255.19. Gat Y, Bachar GN, Zukerman Z, Belenky A, Gorenish M. Physical examination may miss the diagnosis of bilateral varicocele: a comparative study of 4 diagnostic modalities. J Urol. 2004; 172(4 Pt 1):1414–1417.20. Aydos K, Baltaci S, Salih M, Anafarta K, Beduk Y, Gulsoy U. Use of color Doppler sonography in the evaluation of varicoceles. Eur Urol. 1993; 24:221–225.21. Lee J, Binsaleh S, Lo K, Jarvi K. Varicoceles: the diagnostic dilemma. J Androl. 2008; 29:143–146.22. Caskurlu T, Tasci AI, Resim S, Sahinkanat T, Ekerbicer H. Reliability of venous diameter in the diagnosis of subclinical varicocele. Urol Int. 2003; 71:83–86.23. Kocakoc E, Kiris A, Orhan I, Bozgeyik Z, Kanbay M, Ogur E. Incidence and importance of reflux in testicular veins of healthy men evaluated with color duplex sonography. J Clin Ultrasound. 2002; 30:282–287.24. Mihmanli I, Kurugoglu S, Cantasdemir M, Zulfikar Z, Halit Yilmaz M, Numan F. Color Doppler ultrasound in subclinical varicocele: an attempt to determine new criteria. Eur J Ultrasound. 2000; 12:43–48.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scrotal Doppler Ultrasonography in the Assessment of Varicocele
- A Study of Scrotal Scan in the Diagnosis of Varicocele
- An Effects of Repeated Valsalva Maneuver on Circulation of Normal Men
- The Correlation of the Degree of Varicocele with Duplex Doppler Ultrasonographic Diameter of the Pampiniform Plexus and the Retrograde Venous Flow
- Varicocele in Children and Low Teenagers: Studies on Prevalence. Scrotal Temperature and Testicular Volume