J Korean Soc Radiol.
2015 Dec;73(6):384-388. 10.3348/jksr.2015.73.6.384.
Percutaneous Ethanol Sclerotherapy for Recurrent Adventitial Cystic Disease of External Iliac Vein after Surgical Treatment: A Case Report
- Affiliations
-
- 1Department of Radiology, Gachon University Gil Medical Center, Incheon, Korea. ho7ok7@gilhospital.com
- 2Department of Vascular Surgery, Gachon University Gil Medical Center, Incheon, Korea.
- KMID: 2130943
- DOI: http://doi.org/10.3348/jksr.2015.73.6.384
Abstract
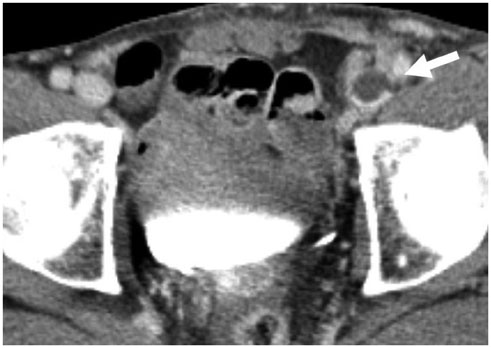
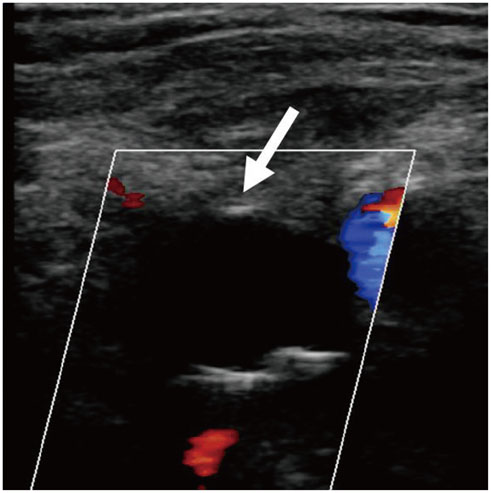
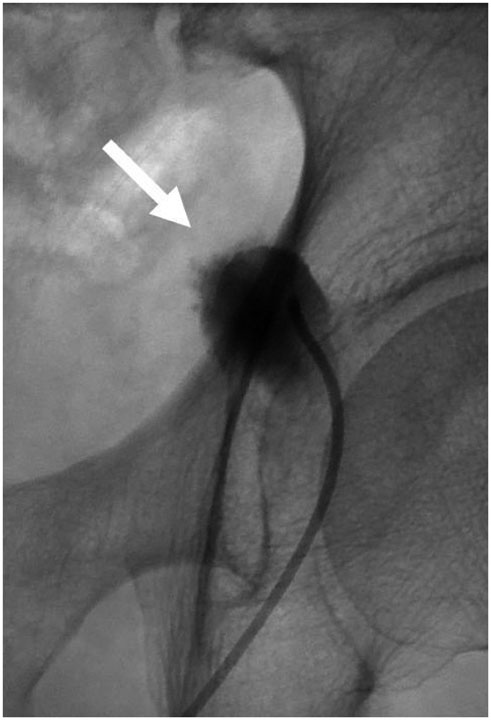
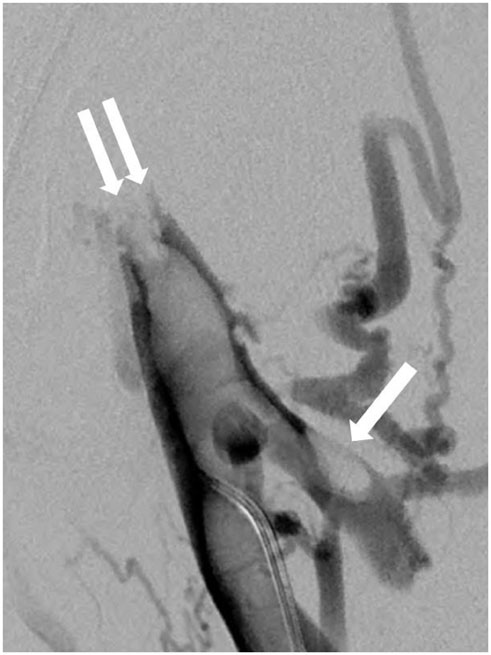
- Adventitial cystic disease (ACD) is a rare, but well-characterized vascular disease. It is most commonly seen in the popliteal artery, but it has also been reported in the venous system. The most commonly involved segment has been the common femoral vein; the disease resulted in luminal compromise and extremity swelling. We report here on a case of percutaneous aspiration and ethanol sclerotherapy for recurrent ACD after surgery of the external iliac vein in a 70-year-old man who presented with a painless swelling of his left leg.
MeSH Terms
Figure
Reference
-
1. Wright LB, Matchett WJ, Cruz CP, James CA, Culp WC, Eidt JF, et al. Popliteal artery disease: diagnosis and treatment. Radiographics. 2004; 24:467–479.2. Lie JT, Jensen PL, Smith RE. Adventitial cystic disease of the lesser saphenous vein. Arch Pathol Lab Med. 1991; 115:946–948.3. Sieunarine K, Lawrence-Brown MM, Kelsey P. Adventitial cystic disease of the popliteal artery: early recurrence after CT guided percutaneous aspiration. J Cardiovasc Surg (Torino). 1991; 32:702–704.4. Johnson JM, Kiankhooy A, Bertges DJ, Morris CS. Percutaneous image-guided aspiration and sclerosis of adventitial cystic disease of the femoral vein. Cardiovasc Intervent Radiol. 2009; 32:812–816.5. Gasparis AP, Wall P, Ricotta JJ. Adventitial cystic disease of the external iliac vein presenting with deep venous thrombosis. A case report. Vasc Endovascular Surg. 2004; 38:273–276.6. Beregi JP, Djabbari M, Desmoucelle F, Willoteaux S, Wattinne L, Louvegny S. Popliteal vascular disease: evaluation with spiral CT angiography. Radiology. 1997; 203:477–483.7. Deutsch AL, Hyde J, Miller SM, Diamond CG, Schanche AF. Cystic adventitial degeneration of the popliteal artery: CT demonstration and directed percutaneous therapy. AJR Am J Roentgenol. 1985; 145:117–118.8. Keo HH, Baumgartner I, Schmidli J, Do DD. Sustained remission 11 years after percutaneous ultrasound-guided aspiration for cystic adventitial degeneration in the popliteal artery. J Endovasc Ther. 2007; 14:264–265.9. di Marzo L, Peetz DJ Jr, Bewtra C, Schultz RD, Feldhaus RJ, Anthone G. Cystic adventitial degeneration of the femoral artery: is evacuation and cyst excision worthwhile as a definitive therapy. Surgery. 1987; 101:587–593.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adventitial Cystic Disease of the External Iliac Vein in a Patient Presenting with Leg Edema
- Adventitial Cystic Disease of the Left External Iliac Vein: A Case Report
- Adventitial Cystic Disease of the Common Femoral Vein Mimicking Deep Venous Thrombosis: A Case Report
- Percutaneous sclerotherapy of varicocele with absolute ethanol
- Adventitial Cystic Disease of the Superficial Femoral Vein without a Joint Connection: A Case Report