Yonsei Med J.
2014 Jul;55(4):904-911. 10.3349/ymj.2014.55.4.904.
Coronary Flow Reserve in the Remote Myocardium Predicts Left Ventricular Remodeling Following Acute Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, The Fourth Affiliated Hospital of Harbin Medical University, Heilongjiang Province, China. lixueqi@ymail.com
- 2Department of Echocardiology, The Second Affiliated Hospital of Harbin Medical University, Heilongjiang Province, China.
- KMID: 2130813
- DOI: http://doi.org/10.3349/ymj.2014.55.4.904
Abstract
- PURPOSE
Coronary flow reserve (CFR) in the non-infarcted myocardium is often impaired following acute myocardial infarction (AMI). However, the clinical significance of CFR in the non-infarcted myocardium is not fully understood. The objective of the present study was to assess whether a relationship exists between CFR and left ventricular remodeling following AMI.
MATERIALS AND METHODS
We enrolled 18 consecutive patients undergoing coronary intervention. Heart function was analyzed using real-time myocardial contrast echocardiography at one week and six months after coronary angioplasty. Ten subjects were enrolled as the control group and were examined using the same method at the same time to assess CFR. Cardiac troponin I (cTnI) levels were routinely analyzed to estimate peak concentration.
RESULTS
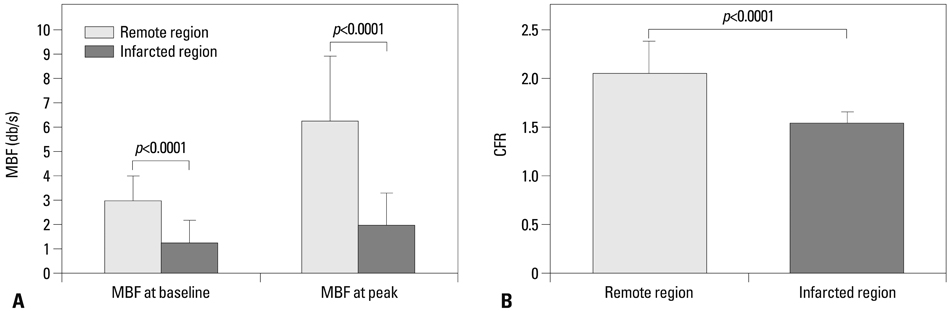
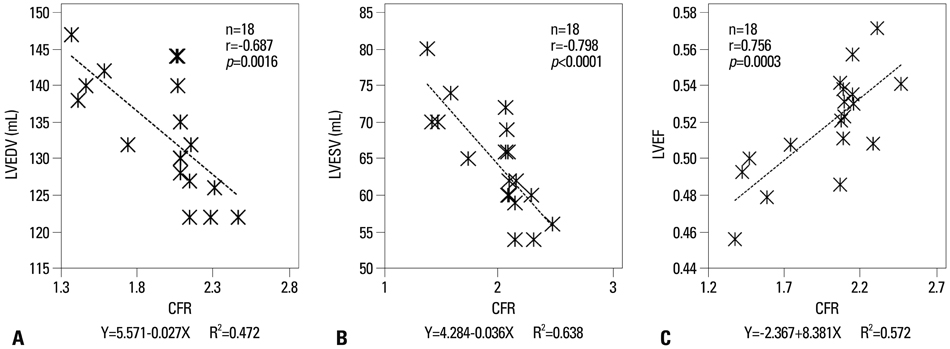
CFR was 1.55+/-0.11 in the infarcted zone and 2.05+/-0.31 in the remote zone (p<0.01) at one week following AMI. According to CFR values in the remote zone, all patients were divided into two groups: Group I (CFR <2.05) and Group II (CFR >2.05). The levels of cTnI were higher in Group I compared to Group II on admission (36.40 vs. 21.38, p<0.05). Furthermore, left ventricular end diastolic volume was higher in Group I compared to Group II at six months following coronary angioplasty.
CONCLUSION
Microvascular dysfunction is commonly observed in the remote myocardium. The CFR value accurately predicts adverse ventricular remodeling following AMI.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic Hypothermia for Cardioprotection in Acute Myocardial Infarction
In Sook Kang, Ikeno Fumiaki, Wook Bum Pyun
Yonsei Med J. 2016;57(2):291-297. doi: 10.3349/ymj.2016.57.2.291.
Reference
-
1. Funaro S, La Torre G, Madonna M, Galiuto L, Scarà A, Labbadia A, et al. Incidence, determinants, and prognostic value of reverse left ventricular remodelling after primary percutaneous coronary intervention: results of the Acute Myocardial Infarction Contrast Imaging (AMICI) multicenter study. Eur Heart J. 2009; 30:566–575.
Article2. Geshi T, Nakano A, Uzui H, Okazawa H, Yonekura Y, Ueda T, et al. Relationship between impaired microvascular function in the non-infarct-related area and left-ventricular remodeling in patients with myocardial infarction. Int J Cardiol. 2008; 126:366–373.
Article3. Bodí V, Sanchis J, Núñez J, López-Lereu MP, Mainar L, Bosch MJ, et al. [Abnormal myocardial perfusion after infarction in patients with persistent TIMI grade-3 flow. Only an acute phenomenon?]. Rev Esp Cardiol. 2007; 60:486–492.
Article4. Pacella JJ, Villanueva FS. Effect of coronary stenosis on adjacent bed flow reserve: assessment of microvascular mechanisms using myocardial contrast echocardiography. Circulation. 2006; 114:1940–1947.
Article5. Laser A, Ingwall JS, Tian R, Reis I, Hu K, Gaudron P, et al. Regional biochemical remodeling in non-infarcted tissue of rat heart post-myocardial infarction. J Mol Cell Cardiol. 1996; 28:1531–1538.
Article6. Wei K. Detection and quantification of coronary stenosis severity with myocardial contrast echocardiography. Prog Cardiovasc Dis. 2001; 44:81–100.
Article7. Mathias W Jr, Kowatsch I, Saroute AN, Osório AF, Sbano JC, Dourado PM, et al. Dynamic changes in microcirculatory blood flow during dobutamine stress assessed by quantitative myocardial contrast echocardiography. Echocardiography. 2011; 28:993–1001.
Article8. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging. 2002; 18:539–542.
Article9. Wita K, Filipecki A, Lelek M, Bochenek T, Elżbieciak M, Wróbel W, et al. Prediction of left ventricular remodeling in patients with STEMI treated with primary PCI: use of quantitative myocardial contrast echocardiography. Coron Artery Dis. 2011; 22:171–178.
Article10. Kurita T, Sakuma H, Onishi K, Ishida M, Kitagawa K, Yamanaka T, et al. Regional myocardial perfusion reserve determined using myocardial perfusion magnetic resonance imaging showed a direct correlation with coronary flow velocity reserve by Doppler flow wire. Eur Heart J. 2009; 30:444–452.
Article11. Armstrong WF, Zoghbi WA. Stress echocardiography: current methodology and clinical applications. J Am Coll Cardiol. 2005; 45:1739–1747.12. Bolognese L, Carrabba N, Parodi G, Santoro GM, Buonamici P, Cerisano G, et al. Impact of microvascular dysfunction on left ventricular remodeling and long-term clinical outcome after primary coronary angioplasty for acute myocardial infarction. Circulation. 2004; 109:1121–1126.
Article13. Lepper W, Hoffmann R, Kamp O, Franke A, de Cock CC, Kühl HP, et al. Assessment of myocardial reperfusion by intravenous myocardial contrast echocardiography and coronary flow reserve after primary percutaneous transluminal coronary angioplasty [correction of angiography] in patients with acute myocardial infarction. Circulation. 2000; 101:2368–2374.
Article14. Anantharam B, Janardhanan R, Hayat S, Hickman M, Chahal N, Bassett P, et al. Coronary flow reserve assessed by myocardial contrast echocardiography predicts mortality in patients with heart failure. Eur J Echocardiogr. 2011; 12:69–75.15. Neizel M, Futterer S, Steen H, Giannitsis E, Reinhardt L, Lossnitzer D, et al. Predicting microvascular obstruction with cardiac troponin T after acute myocardial infarction: a correlative study with contrast-enhanced magnetic resonance imaging. Clin Res Cardiol. 2009; 98:555–562.16. Wita K, Lelek M, Filipecki A, Turski M, Wróbel W, Tabor Z, et al. Microvascular damage prevention with thrombaspiration during primary percutaneous intervention in acute myocardial infarction. Coron Artery Dis. 2009; 20:51–57.17. Coser A, Franchi E, Marini M, Cemin R, Benini A, Beltrame F, et al. Intravenous contrast echocardiography after myocardial infarction: relationship among residual myocardial perfusion, contractile reserve and long-term remodelling. J Cardiovasc Med (Hagerstown). 2007; 8:1012–1019.
Article18. Grayburn PA, Choi JW. Advances in the assessment of no-reflow after successful primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: now that we can diagnose it, what do we do about it? J Am Coll Cardiol. 2008; 51:566–568.
Article19. Park SM, Hong SJ, Kim YH, Ahn CM, Lim DS, Shim WJ. Predicting myocardial functional recovery after acute myocardial infarction: relationship between myocardial strain and coronary flow reserve. Korean Circ J. 2010; 40:639–644.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Myocardial Stunning on Remote Coronary Flow Reserve
- Coronary Flow Reserve in Non-Infarcted Myocardium Predicts Long-Term Clinical Outcomes in Patients Undergoing Percutaneous Coronary Intervention
- Assessment of Myocardial Viability Using PET
- Coronary Flow Velocity Pattern in Patients with Myocardial Bridging of Coronary Artery
- Comparison of TIMI Myocardial Perfusion Grade with Coronary Flow Reserve for Prediction of Recovery of LV Function and LV Remodeling in Acute Myocardial Infarction