J Korean Med Sci.
2014 Aug;29(8):1170-1173. 10.3346/jkms.2014.29.8.1170.
Acute Pancreatitis Induced by Methimazole Treatment in a 51-Year-Old Korean Man: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. jrhahm@hanmail.net
- 2Institute of Health Science, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Department of Laboratory Medicine, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2129616
- DOI: http://doi.org/10.3346/jkms.2014.29.8.1170
Abstract
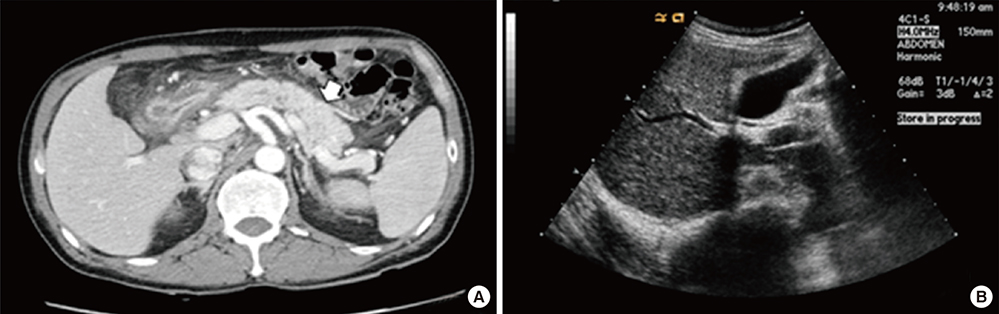
- Methimazole (MMI)-induced acute pancreatitis is very rare but severe adverse reaction. A 51-yr-old male developed a high fever, chills, and abdominal pain, two weeks after commencement on MMI for the treatment of Graves' disease. There was no evidence of agranulocytosis, and fever subsided soon after stopping MMI treatment. However, 5 hr after taking an additional dose of MMI, abdominal pain and fever developed again. His symptoms, biochemical, and imaging studies were compatible with acute pancreatitis. After withdrawal of MMI, he showed clinical improvement. This is the first case of MMI-induced acute pancreatitis in Korea. Clinicians should be aware of the rare but possible MMI-induced pancreatitis in patients complaining of fever and abdominal pain.
MeSH Terms
Figure
Reference
-
1. Cooper DS. Antithyroid drugs. N Engl J Med. 2005; 352:905–917.2. Yang M, Qu H, Deng HC. Acute pancreatitis induced by methimazole in a patient with Graves' disease. Thyroid. 2012; 22:94–96.3. Taguchi M, Yokota M, Koyano H, Endo Y, Ozawa Y. Acute pancreatitis and parotitis induced by methimazole in a patient with Graves' disease. Clin Endocrinol (Oxf). 1999; 51:667–670.4. Abraham A, Raghavan P, Patel R, Rajan D, Singh J, Mustacchia P. Acute pancreatitis induced by methimazole therapy. Case Rep Gastroenterol. 2012; 6:223–231.5. Vinklerová I, Procházka M, Procházka V, Urbánek K. Incidence, severity, and etiology of drug-induced acute pancreatitis. Dig Dis Sci. 2010; 55:2977–2981.6. Trivedi CD, Pitchumoni CS. Drug-induced pancreatitis: an update. J Clin Gastroenterol. 2005; 39:709–716.7. Kawa S, Ota M, Yoshizawa K, Horiuchi A, Hamano H, Ochi Y, Nakayama K, Tokutake Y, Katsuyama Y, Saito S, et al. HLA DRB10405-DQB10401 haplotype is associated with autoimmune pancreatitis in the Japanese population. Gastroenterology. 2002; 122:1264–1269.8. Awata T, Katsuren E, Matsumoto C, Nagayama I, Uchigata Y, Kuzuya N, Kanazawa Y. Absence of shared HLA class II (DR, DQ)-linked genetic basis between IDDM and autoimmune thyroid disease in Japanese. Diabetes Care. 1995; 18:582–583.9. Okazaki K, Uchida K, Koyabu M, Miyoshi H, Takaoka M. Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. J Gastroenterol. 2011; 46:277–288.10. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, Fukushima M, Nikaido T, Nakayama K, Usuda N, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Liver Failure Associated with Methimazole in Patient with Underlying Liver Disease
- A Case of Recurrent Pancreatitis Induced by Trimethoprim-Sulfamethoxazole Re-Exposure
- A Case Report of Methimazole-Induced Acute Liver Failure Successfully Treated with Liver Transplantation
- Acute Pancreatitis Induced by Moringa Oleifera in a 48 years Old Korean Women: A Case Report
- A Case of Acute Pancreatitis Induced by Multiple Drugs in a Patient with Ulcerative Colitis