J Korean Ophthalmol Soc.
2008 Jun;49(6):925-934. 10.3341/jkos.2008.49.6.925.
Results of Trabeculectomy Using Modified Scleral Flap Suture Technique in Comparison with Standard Trabeculectomy
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. jonglee@dankook.ac.kr
- KMID: 2110873
- DOI: http://doi.org/10.3341/jkos.2008.49.6.925
Abstract
-
PURPOSE: To evaluate the efficacy of trabeculectomy using modified scleral flap suture technique
METHODS
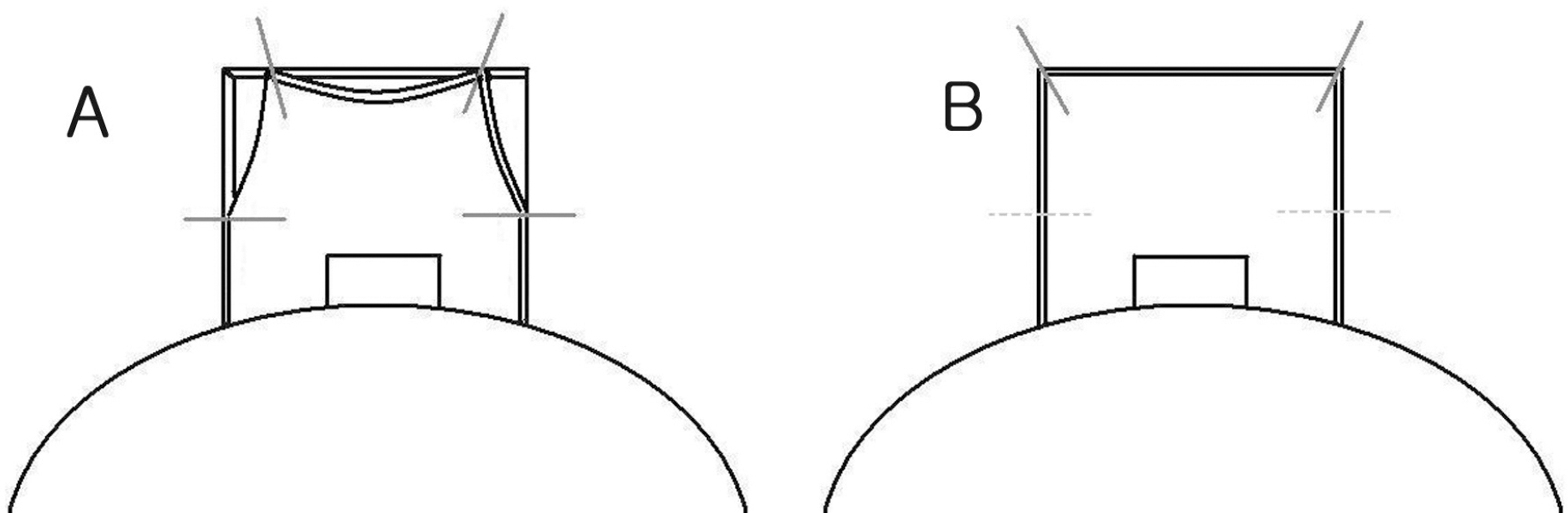
We retrospectively reviewed the medical records of 52 patients (55 eyes) who had undergone trabeculectomy from January 2003 to January 2007. Standard trabeculectomy was performed for 29 eyes of 27 patients, modified trabeculectomy for 26 eyes of 25 patients. We changed suture site of scleral flap corner about 1mm medially from original site and added tight suture to both lateral margins of scleral flap to prevent overflow in modified group. In both groups, most of patients were injected 0.1 ml of 0.02 mg/ml mitomycin-C (MMC) subconjunctivally and the others 0.1 ml of 0.04 mg/ml MMC. We evaluated intraocular pressure (IOP), complication, morphology of filtering bleb, cumulative success rates.
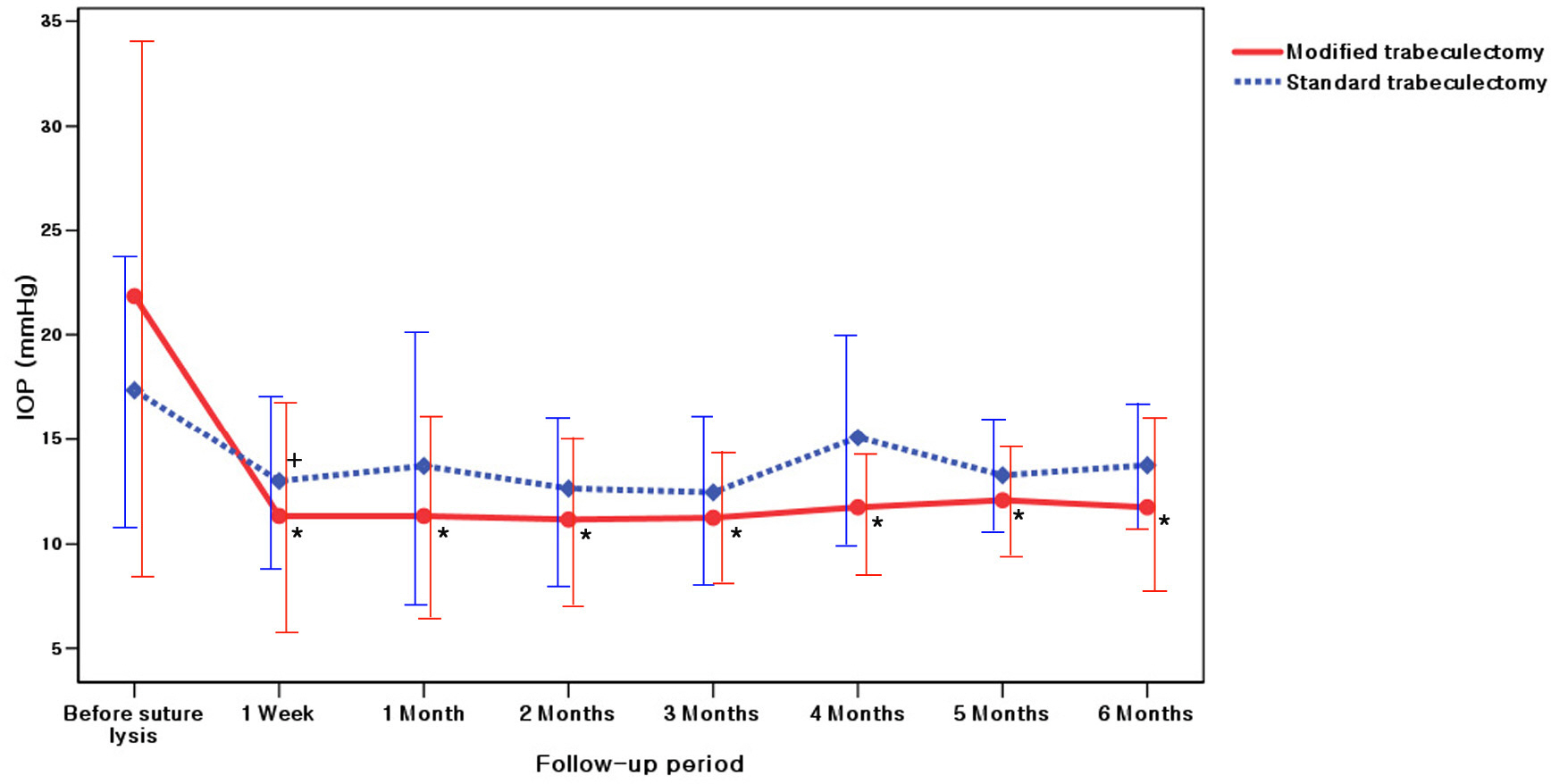
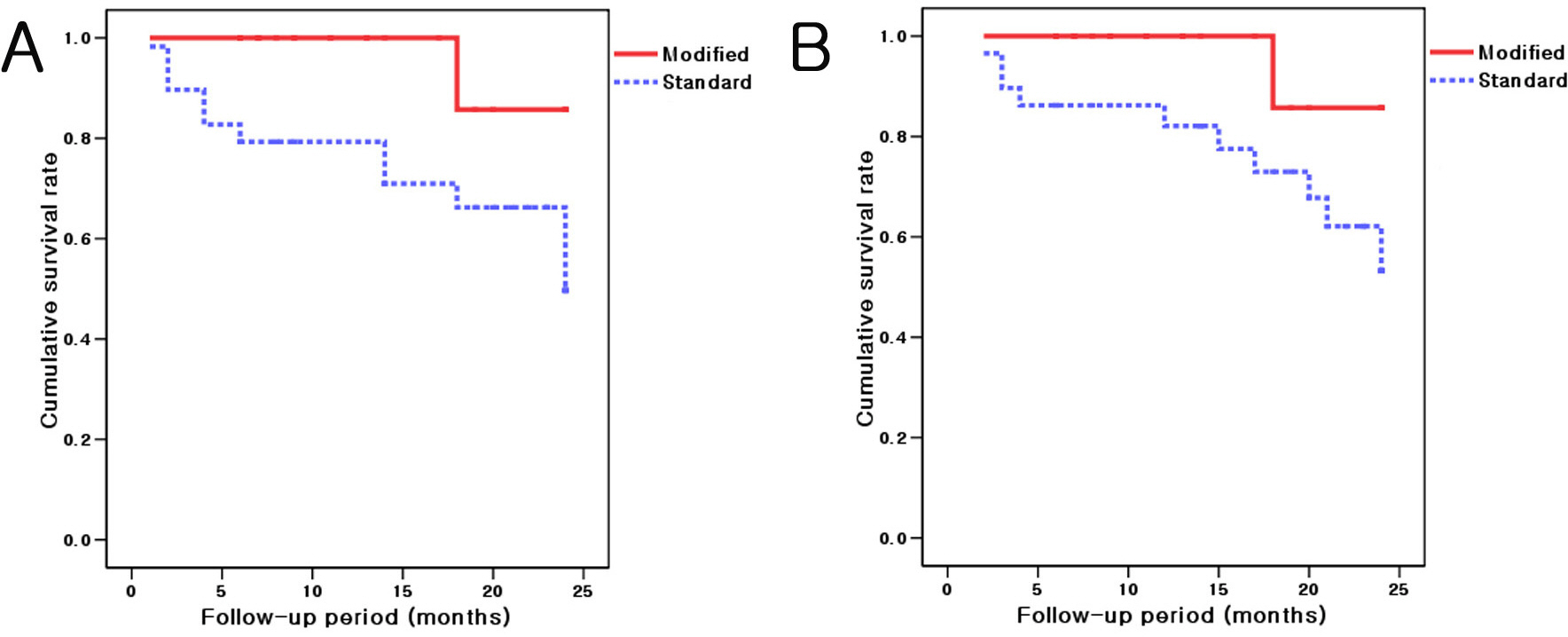
RESULTS
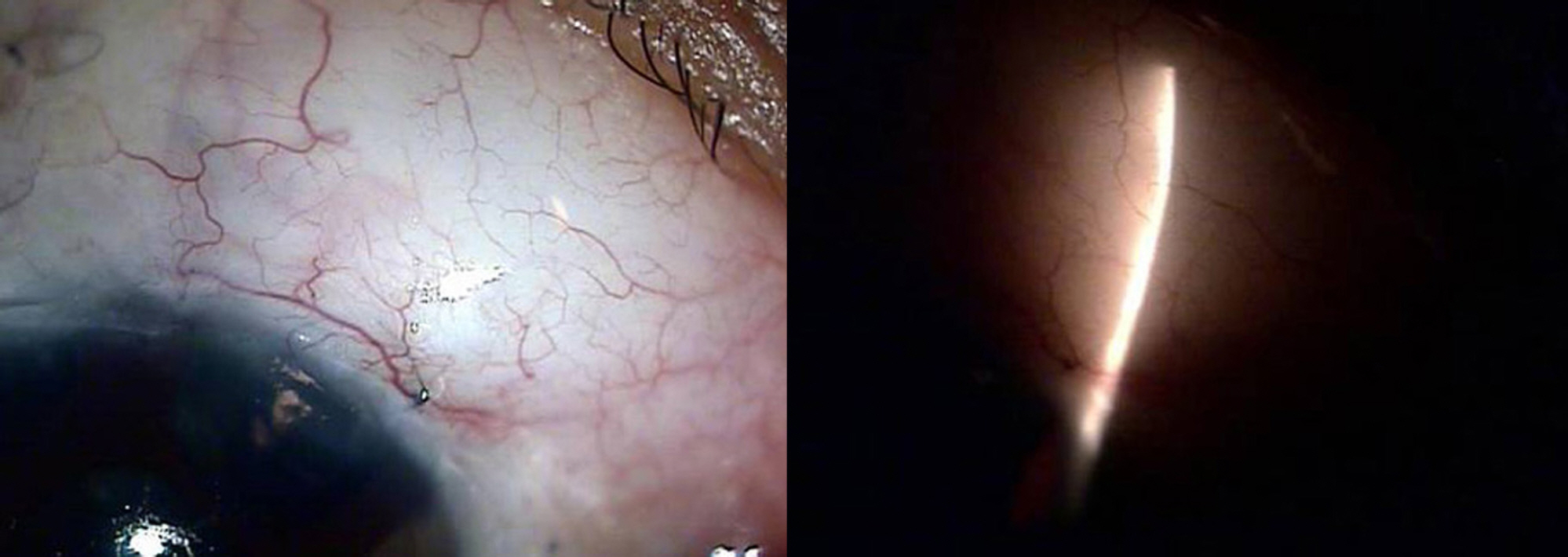
Argon laser suturelysis was performed postoperatively in about half cases of both groups. The IOPs of modified group were consistently lower than those of standard group for 24 months except postoperative 1 day and 1 week. There was a significant difference of IOP at postoperative 2 months and 12 months (p<0.05). No significant difference of complications was found between two groups. The diffuse bleb with microcyst was found in 19 eyes (73%) of modified group and 17 eyes (59%) of standard group. From Kaplan-Meier survival analysis, cumulative success rates of modified group were higher than those of standard group (p<0.05).
CONCLUSIONS
Trabeculectomy using modified scleral flap suture appears to give better IOP control than standard trabeculectomy.
MeSH Terms
Figure
Reference
-
References
1. Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968; 66:673–9.2. Lamping KA, Bellows AR, Hutchinson BT, Afran SI. Long-term evaluation of initial filtration surgery. Ophthalmology. 1986; 93:91–101.
Article3. Akafo SK, Goulstine DB, Rosenthal AR. Long‐ term post trabeculectomy intraocular pressures. Acta Ophthalmol (Copenh). 1992; 70:312–6.4. Bindlish R, Condon GP, Schlosser JD. . Efficacy and safety of mitomycin‐ C in primary trabeculectomy: five‐ year follow‐ up. Ophthalmology. 2002; 109:1336–41.5. WuDunn D, Cantor LB. . A prospective randomized trial comparing intraoperative 5-fluorouracil vs mitomycin C in primary trabeculectomy. Am J Ophthalmol. 2002; 134:521–8.
Article6. Goldenfeld M, Krupin T, Ruderman JM. . 5-Fluorouracil in initial trabeculectomy. A prospective, randomized, multicenter study. Ophthalmology. 1994; 101:1024–9.
Article7. Kim DH, Lee YG, Hong YJ. The Effect of Mitomycin C on Primary Trabeculectomy : Comparative Study in the Same Person. J Korean Ophthalmol Soc. 1998; 39:2129–35.8. Watson PG. Surgery of the glaucomas. Br J Ophthalmol. 1972; 56:299–306.
Article9. Sanders R, MacEwen CJ, Haining WM. Trabeculectomy: effect of varying the surgical site. Eye. 1993; 7:440–3.10. Negi AK, Kiel AW, Vernon SA. Does the site of filtration influence the medium to long term intraocular pressure control following microtrabeculectomy in low risk eyes? Br J Ophthalmol. 2004; 88:1008–11.
Article11. Robin AL, Ramakrishnan R, Krishnadas R. . A long-term dose‐ response study of mitomycin in glaucoma filtration surgery. Arch Ophthalmol. 1997; 115:969–74.12. Sanders SP, Cantor LB, Dobler AA, Hoop JS. Mitomycin C in higher risk trabeculectomy : a prospective comparison of 0.2- to 0.4-mg/cc doses. J Glaucoma. 1999; 8:193–8.13. Kim YY, Sexton RM, Shin DH. . Outcomes of primary phakic trabeculectomies without versus with 0.5- to 1-minute versus 3- to 5-minute mitomycin C. Am J Ophthalmol. 1998; 126:755–62.
Article14. Mietz H, Krieglstein GK. Three‐ year follow-up of trabeculectomies performed with different concentrations of mitomycin‐ C. Ophthalmic Surg Lasers. 1998; 29:628–34.15. Costa VP, Comegno PE, Vasconcelos JP. . Low‐ dose mitomycin C trabeculectomy in patients with advanced glaucoma. J Glaucoma. 1996; 5:193–9.16. Hara T, Araie M, Shirato S, Yamamoto S. Conditions for balance between lower normal pressure control and hypotony in mitomycin trabeculectomy. Graefes Arch Clin Exp Ophthalmol. 1998; 236:420–5.
Article17. Mietz H, Krieglstein GK. Short‐ term clinical results and complications of trabeculectomies performed with mitomycin C using different concentrations. Int Ophthalmol. 1995; 19:51–6.18. Kitazawa Y, Suemori-Matsushita H, Yamamoto T, Kawase K. Low‐ dose and high‐ dose mitomycin trabeculectomy as an initial surgery in primary open-angle glaucoma. Ophthalmology. 1993; 100:1624–8.19. Lee DW, Chang MH, Lee JH. The Comparative Assessment of Filtering Bleb by Timing of subconjunctival Injection of Mitomycin‐ C in Glaucoma Filtering Surgery. J Korean Ophthalmol Soc. 1999; 40:513–22.