J Korean Soc Radiol.
2013 Feb;68(2):99-106. 10.3348/jksr.2013.68.2.99.
CT Findings of Solitary Pulmonary Nodules Less than 8 mm to Differentiate the Malignant and Benign
- Affiliations
-
- 1Department of Radiology, Chonbuk National University Medical School and Hospital, Institute of Medical Science, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, J
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 2097987
- DOI: http://doi.org/10.3348/jksr.2013.68.2.99
Abstract
- PURPOSE
We assessed CT features of the solitary pulmonary nodules (SPNs) smaller than 8 mm to evaluate the differences between the benign and malignant nodules.
MATERIALS AND METHODS
The study included 113 patients (66 male, 47 female, age range: 33-79 years) with SPNs smaller than 8 mm. Mean diameter of SPN on CT was 4.95 +/- 1.19 cm; benign, 4.91 +/- 1.24 mm; and malignant, 6.09 +/- 1.01 mm. Of the 113 nodules, there were 23 (20.4%) malignant nodules and 90 (79.6%) benign nodules. The CT findings (size, shape, margin, density) of SPNs were analyzed. The statistical differences of the malignant and benign nodules were analyzed by chi2 test.
RESULTS
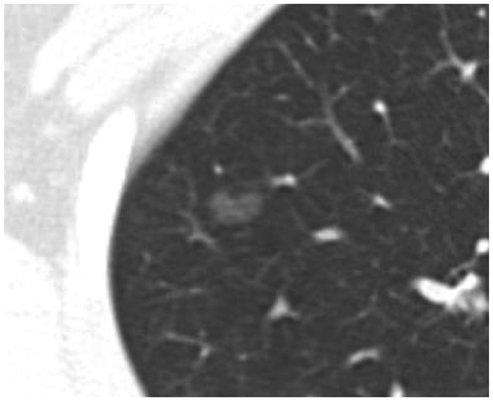
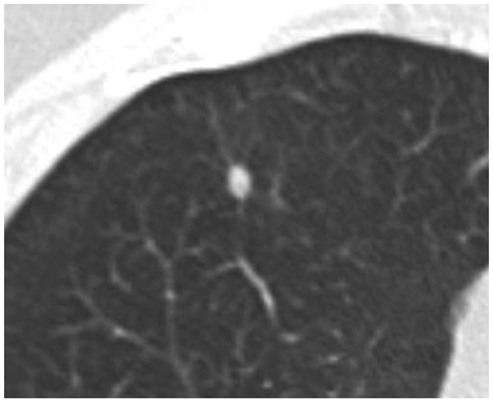
The differences of the benign and malignant nodules were in the margin and density. In the margins, spiculation and lobulation occurred with a significantly higher frequency in the malignant nodules (spiculated: 10/23, lobulated: 7/23) than the benign nodules (spiculated: 20/90, lobulated: 0/90) (p < 0.001). In the mixed or pure ground glass attenuation (14/23), the malignancy rates were significantly higher than the solid nodules (p < 0.001). In the mixed and pure attenuation, a lobulated or spiculated margin (12/14) was associated with a higher risk of malignancy (p = 0.005).
CONCLUSION
In smaller than 8 mm nodules, the predictive CT findings of malignancy were spiculated or lobulated margin and mixed or pure attenuation.
MeSH Terms
Figure
Reference
-
1. Khouri NF, Meziane MA, Zerhouni EA, Fishman EK, Siegelman SS. The solitary pulmonary nodule. Assessment, diagnosis, and management. Chest. 1987. 91:128–133.2. Viggiano RW, Swensen SJ, Rosenow EC 3rd. Evaluation and management of solitary and multiple pulmonary nodules. Clin Chest Med. 1992. 13:83–95.3. Munden RF, Hess KR. "Ditzels" on chest CT: survey of members of the Society of Thoracic Radiology. AJR Am J Roentgenol. 2001. 176:1363–1369.4. Tsukada H, Satou T, Iwashima A, Souma T. Diagnostic accuracy of CT-guided automated needle biopsy of lung nodules. AJR Am J Roentgenol. 2000. 175:239–243.5. vanSonnenberg E, Casola G, Ho M, Neff CC, Varney RR, Wittich GR, et al. Difficult thoracic lesions: CT-guided biopsy experience in 150 cases. Radiology. 1988. 167:457–461.6. Li H, Boiselle PM, Shepard JO, Trotman-Dickenson B, McLoud TC. Diagnostic accuracy and safety of CT-guided percutaneous needle aspiration biopsy of the lung: comparison of small and large pulmonary nodules. AJR Am J Roentgenol. 1996. 167:105–109.7. Bernard A. The Thorax Group. Resection of pulmonary nodules using video-assisted thoracic surgery. Ann Thorac Surg. 1996. 61:202–204. discussion 204-205.8. Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Matsushita T, et al. Small solitary pulmonary nodules (< or =1 cm) detected at population-based CT screening for lung cancer: reliable high-resolution CT features of benign lesions. AJR Am J Roentgenol. 2003. 180:955–964.9. Klein JS, Zarka MA. Transthoracic needle biopsy: an overview. J Thorac Imaging. 1997. 12:232–249.10. Jaklitsch MT, Jacobson FL, Austin JH, Field JK, Jett JR, Keshavjee S, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg. 2012. 144:33–38.11. Wormanns D, Diederich S. Characterization of small pulmonary nodules by CT. Eur Radiol. 2004. 14:1380–1391.12. Lee HJ, Goo JM, Lee CH, Park CM, Kim KG, Park EA, et al. Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol. 2009. 19:552–560.13. Siegelman SS, Khouri NF, Leo FP, Fishman EK, Braverman RM, Zerhouni EA. Solitary pulmonary nodules: CT assessment. Radiology. 1986. 160:307–312.14. Zerhouni EA, Stitik FP, Siegelman SS, Naidich DP, Sagel SS, Proto AV, et al. CT of the pulmonary nodule: a cooperative study. Radiology. 1986. 160:319–327.15. Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999. 354:99–105.16. Munden RF, Pugatch RD, Liptay MJ, Sugarbaker DJ, Le LU. Small pulmonary lesions detected at CT: clinical importance. Radiology. 1997. 202:105–110.17. Proto AV, Thomas SR. Pulmonary nodules studied by computed tomography. Radiology. 1985. 156:149–153.18. Midthun DE, Swensen SJ, Jett JR, Hartman TE. Evaluation of nodules detected by screening for lung cancer with low dose spiral computed tomography. Lung Cancer. 2003. 41:suppl 2. S40.19. Henschke CI, Yankelevitz DF, Naidich DP, McCauley DI, McGuinness G, Libby DM, et al. CT screening for lung cancer: suspiciousness of nodules according to size on baseline scans. Radiology. 2004. 231:164–168.20. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS. ELCAP Group. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002. 178:1053–1057.21. Nakata M, Saeki H, Takata I, Segawa Y, Mogami H, Mandai K, et al. Focal ground-glass opacity detected by low-dose helical CT. Chest. 2002. 121:1464–1467.22. Li F, Sone S, Abe H, Macmahon H, Doi K. Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology. 2004. 233:793–798.23. MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005. 237:395–400.24. Jeudy J, White CS, Munden RF, Boiselle PM. Management of small (3-5-mm) pulmonary nodules at chest CT: global survey of thoracic radiologists. Radiology. 2008. 247:847–853.25. Benjamin MS, Drucker EA, McLoud TC, Shepard JA. Small pulmonary nodules: detection at chest CT and outcome. Radiology. 2003. 226:489–493.26. Henschke CI, Naidich DP, Yankelevitz DF, McGuinness G, McCauley DI, Smith JP, et al. Early lung cancer action project: initial findings on repeat screenings. Cancer. 2001. 92:153–159.27. Piyavisetpat N, Aquino SL, Hahn PF, Halpern EF, Thrall JH. Small incidental pulmonary nodules: how useful is short-term interval CT follow-up? J Thorac Imaging. 2005. 20:5–9.28. Libby DM, Wu N, Lee IJ, Farooqi A, Smith JP, Pasmantier MW, et al. CT screening for lung cancer: the value of short-term CT follow-up. Chest. 2006. 129:1039–1042.