J Korean Soc Radiol.
2013 Feb;68(2):87-97. 10.3348/jksr.2013.68.2.87.
Endovascular Aortic Aneurysm Repair for Abdominal Aortic Aneurysm: Single Center Experience in 122 Patients
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea. apleseed@chol.com
- 2Department of Radiology, Chonnam National University Hwasun Hospital, Chonnam National University School of Medicine, Hwasun, Korea.
- 3Department of Surgery, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea.
- KMID: 2097986
- DOI: http://doi.org/10.3348/jksr.2013.68.2.87
Abstract
- PURPOSE
To analyze a single center experience of endovascular aneurysm repair (EVAR) for abdominal aortic aneurysms.
MATERIALS AND METHODS
Results of 122 patients who underwent EVAR were analyzed, retrospectively. Sex, age, aneurysmal morphology, hostile neck anatomy, preprocedural and postprocedural sac-diameter, technical and clinical success, postprocedural complication and need of additional procedure were analyzed.
RESULTS
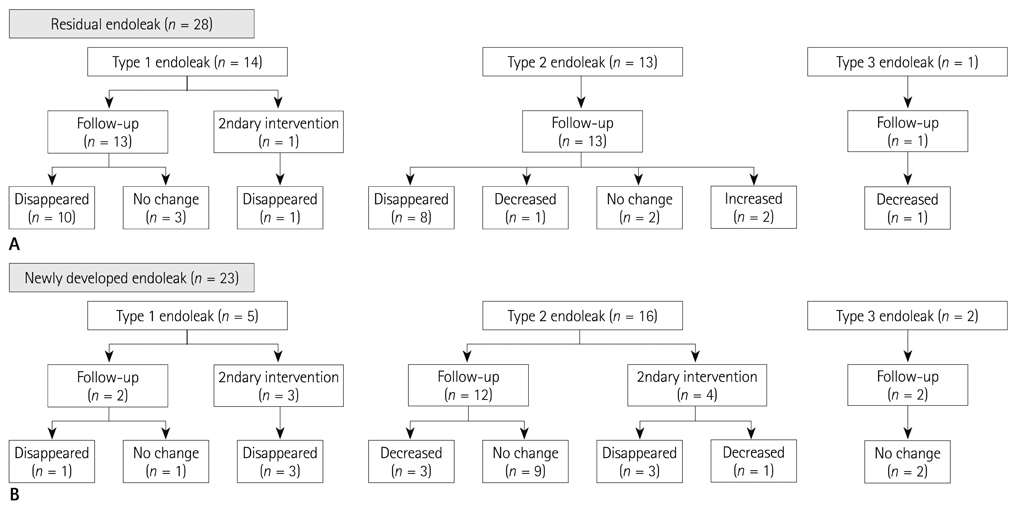
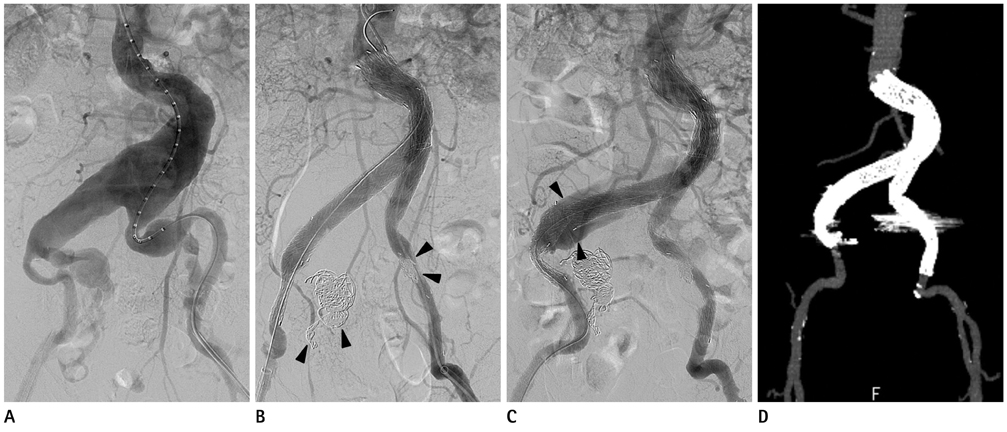
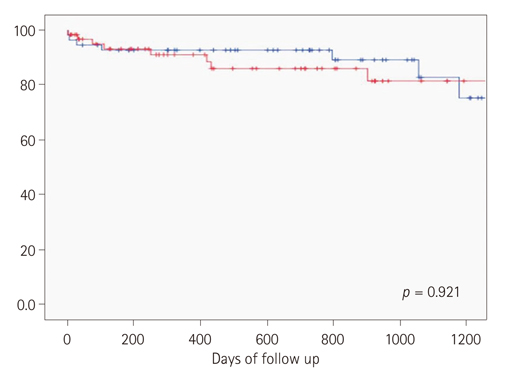
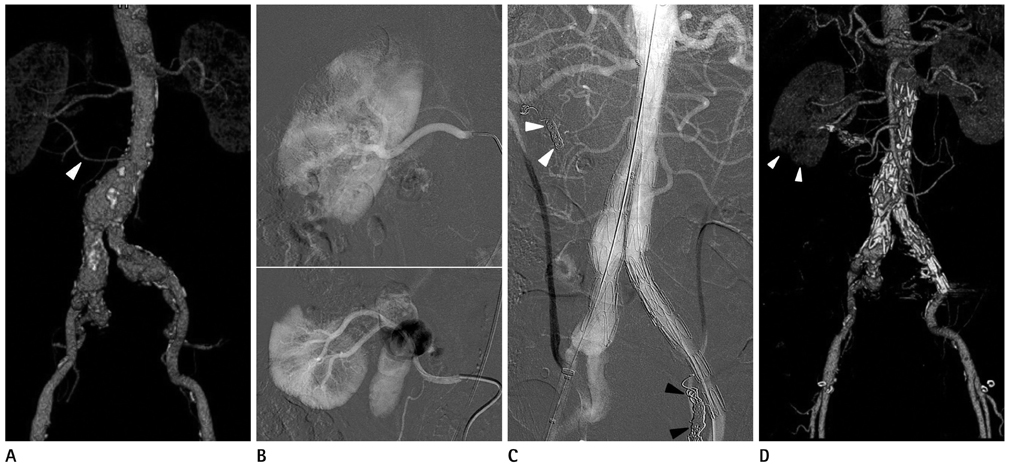
A total of 111 male and 11 female patients were included. Morphology of the aneurysms was as follows: fusiform (n = 108), saccular (n = 3) and ruptured type (n = 11). Sixty-four patients had hostile neck anatomy. The preprocedural mean sac-diameter was 52.4 mm. Postprocedural sac-diameter was decreased or stable in 110 patients (90.2%) and increased in 8 patients (6.6%). Technical success rate was 100% and clinical success rate was 86.1%. Fifty-one patients showed endoleak (41.8%) and 15 patients (12.3%) underwent secondary intervention due to type I endoleak (n = 4), type II endoleak (n = 4) and stent-graft thrombosis (n = 7).
CONCLUSION
EVAR is a safe and effective therapy for abdominal aortic aneurysm, and it has high technical success and clinical success rate, and low complication rate.
MeSH Terms
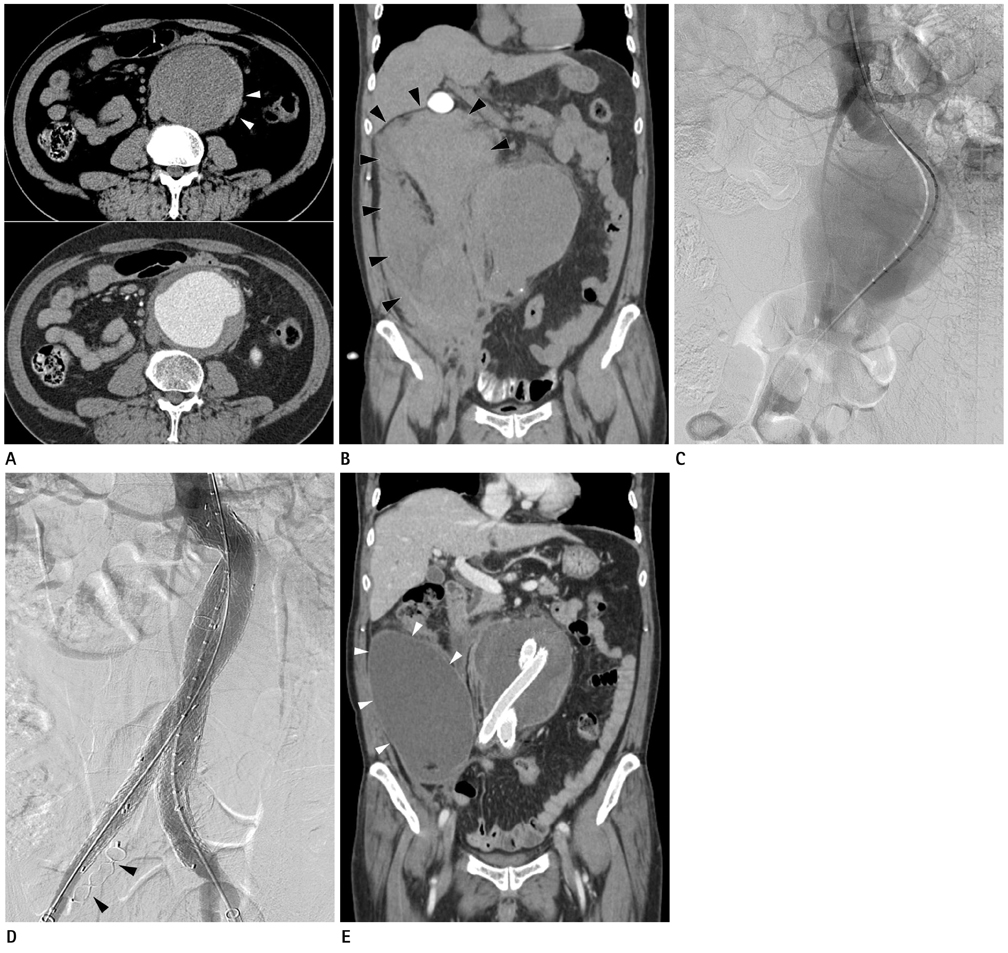
Figure
Reference
-
1. Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991. 5:491–499.2. Kim YW, Min SK, Koh YB, Kim SN, Park JS, Moon IS, et al. Report of nation-wide questionnaire survey for abdominal aortic aneurysm treatment in Korea. J Korean Soc Vasc Surg. 2005. 21:10–15.3. Park YJ, Kim N, Kim YW. Investigation of current trend of AAA treatment in Korea. J Korean Surg Soc. 2011. 80:125–130.4. Prinssen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, Balm R, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004. 351:1607–1618.5. Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG. EVAR trial participants. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 2004. 364:843–848.6. Uflacker R, Robison JG, Brothers TE, Pereira AH, Sanvitto PC. Abdominal aortic aneurysm treatment: preliminary results with the Talent stent-graft system. J Vasc Interv Radiol. 1998. 9(1 Pt 1):51–60.7. Brewster DC, Jones JE, Chung TK, Lamuraglia GM, Kwolek CJ, Watkins MT, et al. Long-term outcomes after endovascular abdominal aortic aneurysm repair: the first decade. Ann Surg. 2006. 244:426–438.8. Chaikof EL, Fillinger MF, Matsumura JS, Rutherford RB, White GH, Blankensteijn JD, et al. Identifying and grading factors that modify the outcome of endovascular aortic aneurysm repair. J Vasc Surg. 2002. 35:1061–1066.9. Veith FJ, Baum RA, Ohki T, Amor M, Adiseshiah M, Blankensteijn JD, et al. Nature and significance of endoleaks and endotension: summary of opinions expressed at an international conference. J Vasc Surg. 2002. 35:1029–1035.10. White GH, Yu W, May J. Endoleak--a proposed new terminology to describe incomplete aneurysm exclusion by an endoluminal graft. J Endovasc Surg. 1996. 3:124–125.11. White GH, May J, Waugh RC, Chaufour X, Yu W. Type III and type IV endoleak: toward a complete definition of blood flow in the sac after endoluminal AAA repair. J Endovasc Surg. 1998. 5:305–309.12. White GH, Yu W, May J, Chaufour X, Stephen MS. Endoleak as a complication of endoluminal grafting of abdominal aortic aneurysms: classification, incidence, diagnosis, and management. J Endovasc Surg. 1997. 4:152–168.13. Henretta JP, Hodgson KJ, Mattos MA, Karch LA, Hurlbert SN, Sternbach Y, et al. Feasibility of endovascular repair of abdominal aortic aneurysms with local anesthesia with intravenous sedation. J Vasc Surg. 1999. 29:793–798.14. Teh LG, Sieunarine K, van Schie G, Goodman MA, Lawrence-Brown M, Prendergast FJ, et al. Use of the percutaneous vascular surgery device for closure of femoral access sites during endovascular aneurysm repair: lessons from our experience. Eur J Vasc Endovasc Surg. 2001. 22:418–423.15. Jung HD, Lee YY, Lee SJ, Lim JH, Yim NY, Chang NK, et al. Outcomes and prognostic factors of endovascular abdominal aortic aneurysm repair in patients with hostile neck anatomy. J Korean Soc Radiol. 2012. 67:323–332.16. Buth J, Harris PL, van Marrewijk C, Fransen G. The significance and management of different types of endoleaks. Semin Vasc Surg. 2003. 16:95–102.17. Jones JE, Atkins MD, Brewster DC, Chung TK, Kwolek CJ, LaMuraglia GM, et al. Persistent type 2 endoleak after endovascular repair of abdominal aortic aneurysm is associated with adverse late outcomes. J Vasc Surg. 2007. 46:1–8.18. Bernhard VM, Mitchell RS, Matsumura JS, Brewster DC, Decker M, Lamparello P, et al. Ruptured abdominal aortic aneurysm after endovascular repair. J Vasc Surg. 2002. 35:1155–1162.19. Aquino RV, Rhee RY, Muluk SC, Tzeng EY, Carrol NM, Makaroun MS. Exclusion of accessory renal arteries during endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 2001. 34:878–884.20. Kim B, Donayre CE, Hansen CJ, Aziz I, Walot I, Lippmann M, et al. Endovascular abdominal aortic aneurysm repair using the AneuRx stent graft: impact of excluding accessory renal arteries. Ann Vasc Surg. 2004. 18:32–37.21. Karmacharya J, Parmer SS, Antezana JN, Fairman RM, Woo EY, Velazquez OC, et al. Outcomes of accessory renal artery occlusion during endovascular aneurysm repair. J Vasc Surg. 2006. 43:8–13.22. Greenberg R, Fairman R, Srivastava S, Criado F, Green R. Endovascular grafting in patients with short proximal necks: an analysis of short-term results. Cardiovasc Surg. 2000. 8:350–354.23. Choke E, Munneke G, Morgan R, Belli AM, Loftus I, McFarland R, et al. Outcomes of endovascular abdominal aortic aneurysm repair in patients with hostile neck anatomy. Cardiovasc Intervent Radiol. 2006. 29:975–980.24. Verhoeven EL, Tielliu IF, Muhs BE, Bos WT, Zeebregts CJ, Prins TR, et al. Fenestrated and branched stent-grafting: a 5-years experience. Acta Chir Belg. 2006. 106:317–322.25. Park JH, Chung JW, Choo IW, Kim SJ, Lee JY, Han MC. Fenestrated stent-grafts for preserving visceral arterial branches in the treatment of abdominal aortic aneurysms: preliminary experience. J Vasc Interv Radiol. 1996. 7:819–823.26. Scurr JR, Brennan JA, Gilling-Smith GL, Harris PL, Vallabhaneni SR, McWilliams RG. Fenestrated endovascular repair for juxtarenal aortic aneurysm. Br J Surg. 2008. 95:326–332.27. Ohrlander T, Sonesson B, Ivancev K, Resch T, Dias N, Malina M. The chimney graft: a technique for preserving or rescuing aortic branch vessels in stent-graft sealing zones. J Endovasc Ther. 2008. 15:427–432.28. Jeong SI, Jung HD, Lim JH, Yim NY, Chang NK, Kim JK, et al. A case report of the endovascular treatment of mycotic abdominal aortic pseudoaneurysms using a customized stent-graft. J Korean Soc Radiol. 2011. 65:241–245.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Abdominal Aortic Aneurysm with Antecedent Endovascular Repair of Abdominal Aortic Aneurysm
- Abdominal Aortic Aneurysm
- Endovascular Repair of a Juxtarenal Abdominal Aortic Aneurysm Using a Chimney Graft
- The Complications and Their Management after Endovascular Aneurysm Repair for the Treatment of Abdominal Aortic Aneurysms
- Endovascular Stent-Graft Placement and Secondary Intervention for Abdominal Aortic Aneurysm in a Patient who had a Previously Inserted Iliac Stent