J Korean Surg Soc.
2011 Jun;80(Suppl 1):S67-S70. 10.4174/jkss.2011.80.Suppl1.S67.
Experience of non-vascular complications following endovascular aneurysm repair for abdominal aortic aneurysm
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. imjung@brm.co.kr
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Eulji University College of Medicine, Daejon, Korea.
- 4Department of Surgery, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- KMID: 2096655
- DOI: http://doi.org/10.4174/jkss.2011.80.Suppl1.S67
Abstract
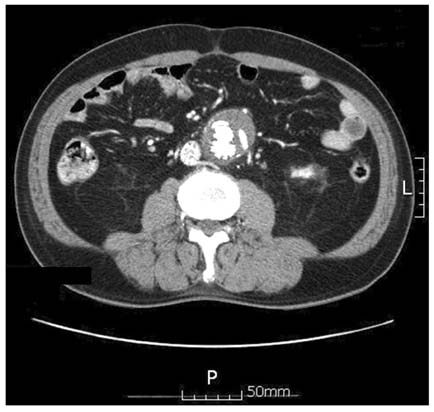
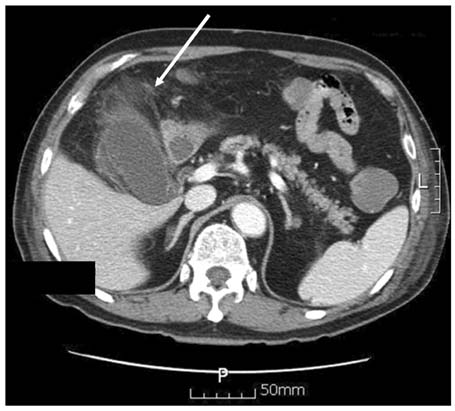
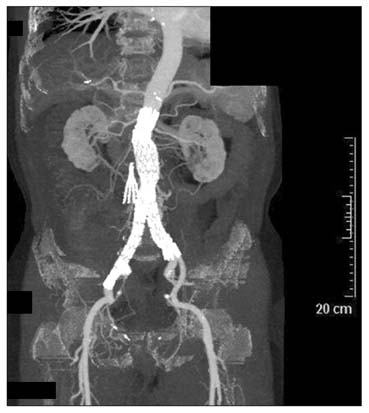
- Endovascular aneurysm repair (EVAR) for the treatment of abdominal aortic aneurysm (AAA) is a widely used method, and its decreased invasiveness compared to traditional surgical repair has brought about reduced rates of morbidity and mortality. Several vascular complications related to the procedure have been reported, but non-vascular complications have rarely occurred. We report herein the case of a 78-year-old man who underwent EVAR for AAA and presented with active duodenal ulcer bleeding and acute acalculous cholecystitis as complications after the procedure. We must consider that a wide spectrum of complications may occur following EVAR, and therefore it is important to evaluate the risks of complication and to take the necessary measures to minimize them.
MeSH Terms
Figure
Reference
-
1. Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al. Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model. Health Technol Assess. 2009. 13:1–189. 215–318. iii2. Drury D, Michaels JA, Jones L, Ayiku L. Systematic review of recent evidence for the safety and efficacy of elective endovascular repair in the management of infrarenal abdominal aortic aneurysm. Br J Surg. 2005. 92:937–946.3. Becquemin JP, Allaire E, Desgranges P, Kobeiter H. Delayed complications following EVAR. Tech Vasc Interv Radiol. 2005. 8:30–40.4. Ruby BJ, Cogbill TH. Aortoduodenal fistula 5 years after endovascular abdominal aortic aneurysm repair with the Ancure stent graft. J Vasc Surg. 2007. 45:834–836.5. Berg P, Kaufmann D, van Marrewijk CJ, Buth J. Spinal cord ischaemia after stent-graft treatment for infra-renal abdominal aortic aneurysms: analysis of the Eurostar database. Eur J Vasc Endovasc Surg. 2001. 22:342–347.6. James AD, Anderson HJ, Edwards R, Sandison AJ. Pancreatitis as a complication of endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2008. 35:310–311.7. Fidler F, Prosek V. Acute acalculous cholecystitis as a postoperative complication: the stress gallbladder. Rozhl Chir. 1991. 70:495–497.8. Schirren J, Dietz W, Rothmund M. Acute acalculous cholecystitis: a stress-induced complication. Chirurg. 1990. 61:382–386.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Abdominal Aortic Aneurysm with Antecedent Endovascular Repair of Abdominal Aortic Aneurysm
- The Complications and Their Management after Endovascular Aneurysm Repair for the Treatment of Abdominal Aortic Aneurysms
- Acute Type B Aortic Dissection in a Patient with Previous Endovascular Abdominal Aortic Aneurysm Repair
- Current Endovascular Treatment of Abdominal Aortic Aneurysm
- Novel Technique to Rescue a Folded Aortic Endograft during Endovascular Aneurysm Repair