Ann Surg Treat Res.
2015 Nov;89(5):278-283. 10.4174/astr.2015.89.5.278.
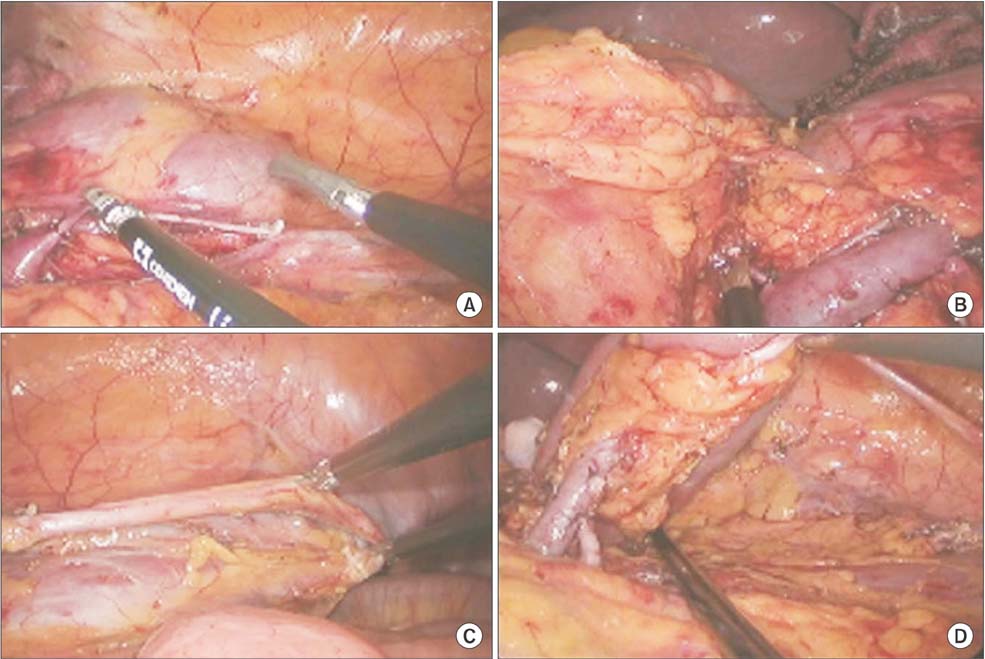
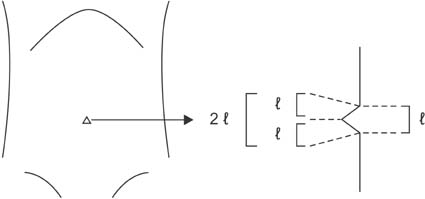
Transumbilical pure single-port laparoscopic donor nephrectomy
- Affiliations
-
- 1Department of Surgery, Daejeon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Daejeon, Korea. zambo9@catholic.ac.kr
- 2Department of Urology, Daejeon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Daejeon, Korea.
- KMID: 2095535
- DOI: http://doi.org/10.4174/astr.2015.89.5.278
Abstract
- Transumbilical single-port laparoscopic donor nephrectomy (SPLDN) is a novel, rapidly evolving, minimally invasive treatment modality for kidney transplantation. This method causes minimal parietal injury, has cosmetic advantages, and allows rapid recovery because of low postoperative pain and short hospital stay. Like other abdominal surgeries, when conducted by experienced laparoscopic surgeons, it can meet the same graft requirements as conventional laparoscopic surgery. Here, we report the first two cases of transumbilical SPLDN at Daejeon St. Mary's Hospital, The Catholic University of Korea. We used the umbilicus as a common path for laparoscopic procedures and as a route for specimen retrieval. The operating times were 230 and 265 minutes in cases 1 and 2, respectively. No intra- or postoperative complications were noted. In case 1, the wound length was 4 cm and duration of hospitalization was 2 days. In case 2, the wound length was only 2.5 cm, and the duration of hospitalization was only 1 day.
MeSH Terms
Figure
Reference
-
1. Ramasamy R, Afaneh C, Katz M, Chen X, Aull MJ, Leeser DB, et al. Comparison of complications of laparoscopic versus laparoendoscopic single site donor nephrectomy using the modified Clavien grading system. J Urol. 2011; 186:1386–1390.2. Afaneh C, Aull MJ, Gimenez E, Wang G, Charlton M, Leeser DB, et al. Comparison of laparoendoscopic single-site donor nephrectomy and conventional laparoscopic donor nephrectomy: donor and recipient outcomes. Urology. 2011; 78:1332–1337.3. Kaouk JH, Khalifeh A, Laydner H, Autorino R, Hillyer SP, Panumatrassamee K, et al. Transvaginal hybrid natural orifice transluminal surgery robotic donor nephrectomy: first clinical application. Urology. 2012; 80:1171–1175.4. Kaouk JH, Autorino R. Laparoendoscopic single-site surgery (LESS) and nephrectomy: current evidence and future perspectives. Eur Urol. 2012; 62:613–615.5. Lunsford KE, Harris MT, Nicoll KN, Collins BH, Sudan DL, Kuo PC, et al. Single-site laparoscopic living donor nephrectomy offers comparable perioperative outcomes to conventional laparoscopic living donor nephrectomy at a higher cost. Transplantation. 2011; 91:e16–e17.6. Kok NF, Lind MY, Hansson BM, Pilzecker D, Mertens zur Borg IR, Knipscheer BC, et al. Comparison of laparoscopic and mini incision open donor nephrectomy: single blind, randomised controlled clinical trial. BMJ. 2006; 333:221.7. Simforoosh N, Basiri A, Tabibi A, Shakhssalim N, Hosseini Moghaddam SM. Comparison of laparoscopic and open donor nephrectomy: a randomized controlled trial. BJU Int. 2005; 95:851–855.8. Meng MV, Freise CE, Kang SM, Duh QY, Stoller ML. Techniques to optimize vascular control during laparoscopic donor nephrectomy. Urology. 2003; 61:93–97.9. Canes D, Berger A, Aron M, Brandina R, Goldfarb DA, Shoskes D, et al. Laparoendoscopic single site (LESS) versus standard laparoscopic left donor nephrectomy: matched-pair comparison. Eur Urol. 2010; 57:95–101.10. Barth RN, Phelan MW, Goldschen L, Munivenkatappa RB, Jacobs SC, Bartlett ST, et al. Single-port donor nephrectomy provides improved patient satisfaction and equivalent outcomes. Ann Surg. 2013; 257:527–533.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transumbilical Laparoscopic Cholecystectomy with Additional Port: A Single Surgeon's Experience with 291 Cases
- Single port transumbilical total laparoscopic hysterectomy (TLH): initial experience in Korea
- Transumbilical single port total laparoscopic hysterectomy
- Transumbilical Laparoscopic Assisted Single Port Appendectomy (Hybrid Appendectomy) in Children
- A Case of Single Port Laparoscopic Appendectomy and Cholecystectomy in a Fresh Cadaver: A Feasible Procedure