Korean Circ J.
2010 Mar;40(3):103-111. 10.4070/kcj.2010.40.3.103.
Hybrid Palliation for Neonates With Hypoplastic Left Heart Syndrome: Current Strategies and Outcomes
- Affiliations
-
- 1Division of Cardiovascular Surgery, Hospital for Sick Children, Toronto, Ontario, Canada. christopher.caldarone@sickkids.ca
- KMID: 2094068
- DOI: http://doi.org/10.4070/kcj.2010.40.3.103
Abstract
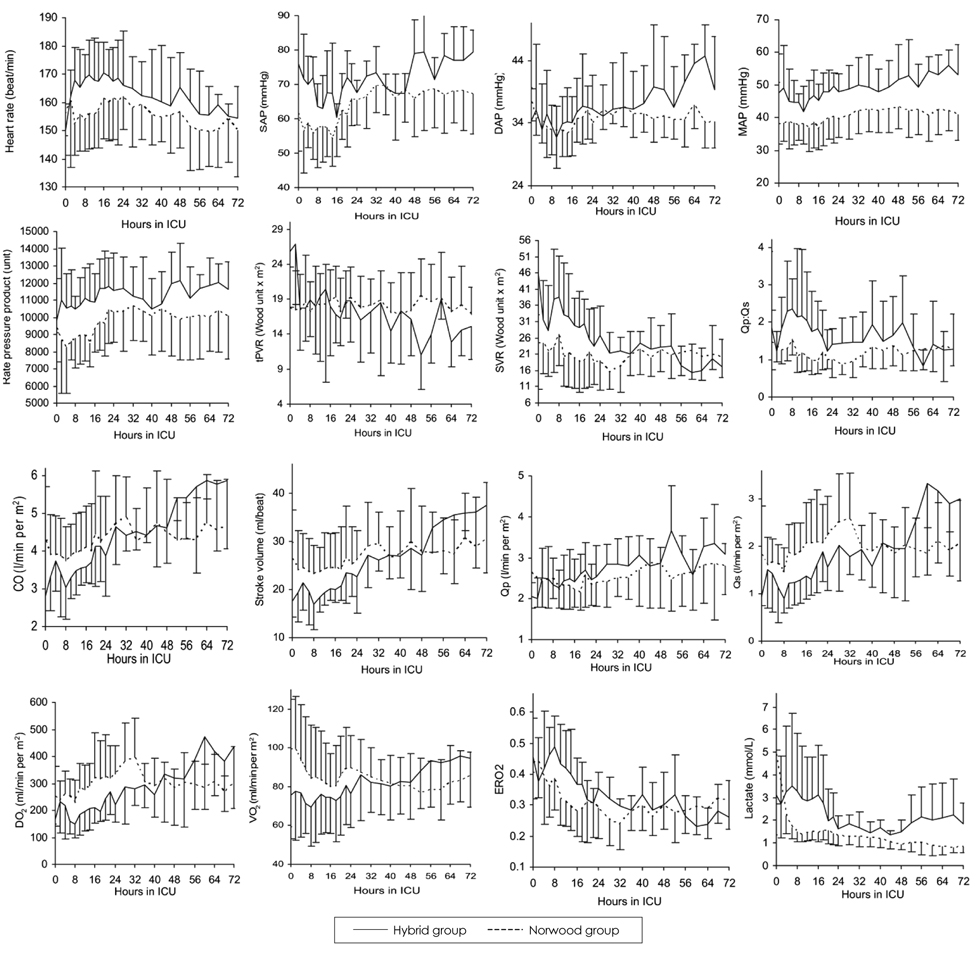
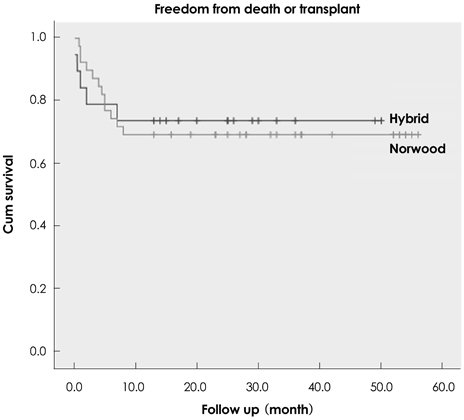
- In the last decade the hybrid procedure has emerged as an alternative stage I palliation in neonates with hypoplastic left heart syndrome (HLHS). This review discusses the historical aspect, surgical and interventional techniques, current outcomes and future direction of this procedure. Hybrid palliation yields equivalent but not superior stage I palliation survival and comparable 1-year survival to conventional Norwood palliation, comparable prestage II hemodynamics and pulmonary artery growth, and preserved ventricular function in stage II palliation. Hybrid palliation utilizes significantly less resource and shortens postoperative recovery. In comprehensive stage II palliation the impact of pulmonary artery reconstruction on subsequent pulmonary artery growth has not been determined and should be further investigated. A prospective, randomized trial is warranted to compare these two surgical strategies for neonates with hypoplastic left heart syndrome.
MeSH Terms
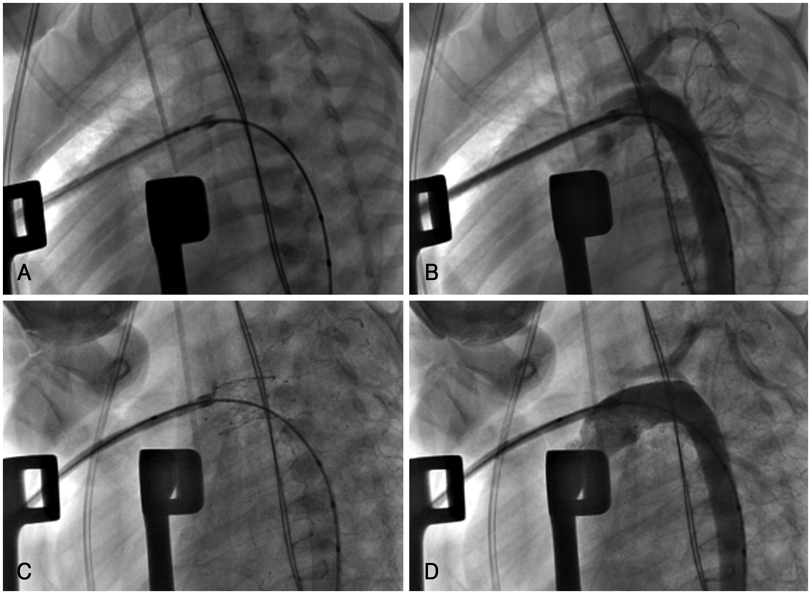
Figure
Reference
-
1. Noonan JA, Nadas AS. The hypoplastic left heart syndrome: an analysis of 101 cases. Pediatr Clin North Am. 1958. 5:1029–1056.2. Norwood WI, Lang P, Hansen DD. Physiologic repair of aortic atresia-hypoplastic left heart syndrome. N Engl J Med. 1983. 308:23–26.3. Mahle WT, Spray TL, Wernovsky G, Gaynor JW, Clark BJ 3rd. Survival after reconstructive surgery for hypoplastic left heart syndrome: a 15-year experience from a single institution. Circulation. 2000. 102:19 Suppl 3. III136–III141.4. De Oliveira NC, Ashburn DA, Khalid F, et al. Prevention of early sudden circulatory collapse after the Norwood operation. Circulation. 2004. 110:11 Suppl 1. II133–II138.5. Stasik CN, Gelehrter S, Goldberg CS, Bove EL, Devaney EJ, Ohye RG. Current outcomes and risk factors for the Norwood procedure. J Thorac Cardiovasc Surg. 2006. 131:412–417.6. Goldberg CS, Schwartz EM, Brunberg JA, et al. Neurodevelopmental outcome of patients after the fontan operation: a comparison between children with hypoplastic left heart syndrome and other functional single ventricle lesions. J Pediatr. 2000. 137:646–652.7. Galli KK, Zimmerman RA, Jarvik GP, et al. Periventricular leukomalacia is common after neonatal cardiac surgery. J Thorac Cardiovasc Surg. 2004. 127:692–704.8. Caldarone CA, Benson L, Holtby H, Li J, Redington AN, Van Arsdell GS. Initial experience with hybrid palliation for neonates with single-ventricle physiology. Ann Thorac Surg. 2007. 84:1294–1300.9. Galantowicz M, Cheatham JP. Lessons learned from the development of a new hybrid strategy for the management of hypoplastic left heart syndrome. Pediatr Cardiol. 2005. 26:190–199.10. Akintuerk H, Michel-Behnke I, Valeske K, et al. Stenting of the arterial duct and banding of the pulmonary arteries: basis for combined Norwood stage I and II repair in hypoplastic left heart. Circulation. 2002. 105:1099–1103.11. Bacha EA, Daves S, Hardin J, et al. Single-ventricle palliation for high-risk neonates: the emergence of an alternative hybrid stage I strategy. J Thorac Cardiovasc Surg. 2006. 131:163–171. e212. Lang P, Norwood WI. Hemodynamic assessment after palliative surgery for hypoplastic left heart syndrome. Circulation. 1983. 68:104–108.13. Pizarro C, Norwood WI. Pulmonary artery banding before Norwood procedure. Ann Thorac Surg. 2003. 75:1008–1010.14. Coe JY, Olley PM. A novel method to maintain ductus arteriosus patency. J Am Coll Cardiol. 1991. 18:837–841.15. Gibbs JL, Wren C, Watterson KG, Hunter S, Hamilton JR. Stenting of the arterial duct combined with banding of the pulmonary arteries and atrial septectomy or septostomy: a new approach to palliation for the hypoplastic left heart syndrome. Br Heart J. 1993. 69:551–555.16. Gibbs JL, Uzun O, Blackburn ME, Wren C, Hamilton JR, Watterson KG. Fate of the stented arterial duct. Circulation. 1999. 99:2621–2625.17. Ruiz CE, Gamra H, Zhang HP, Garcia EJ, Boucek MM. Brief report: stenting of the ductus arteriosus as a bridge to cardiac transplantation in infants with the hypoplastic left-heart syndrome. N Engl J Med. 1993. 328:1605–1608.18. Mitchell MB, Campbell DN, Boucek MM, et al. Mechanical limitation of pulmonary blood flow facilitates heart transplantation in older infants with hypoplastic left heart syndrome. Eur J Cardiothorac Surg. 2003. 23:735–742.19. Galantowicz M, Cheatham JP, Phillips A, et al. Hybrid approach for hypoplastic left heart syndrome: intermediate results after the learning curve. Ann Thorac Surg. 2008. 85:2063–2070. discussion 2070-1.20. Caldarone CA, Benson LN, Holtby H, Van Arsdell GS. Main pulmonary artery to innominate artery shunt during hybrid palliation of hypoplastic left heart syndrome. J Thorac Cardiovasc Surg. 2005. 130:e1–e2.21. Stoica S, Philips A, Egan M, et al. The Retrograde Aortic Arch in the Hybrid Approach to Hypoplastic Left Heart Syndrome Society for Thoracic Surgeons 45th Annual Meeting. 2009. San Fransicsio.22. Li J, Zhang G, Benson L, et al. Comparison of the profiles of postoperative systemic hemodynamics and oxygen transport in neonates after the hybrid or the Norwood procedure: a pilot study. Circulation. 2007. 116:11 Suppl. I179–I187.23. Caldarone CA, Honjo O, Benson LN, Van Arsdell GS. Modification of stage II procedure after hybrid palliation (bilateral pulmonary artery banding and ductal stenting) for hypoplastic left-sided heart syndrome: modified arch reconstruction with retained stented ductus patch. J Thorac Cardiovasc Surg. 2007. 134:1588–1589.24. Li J, Zhang G, McCrindle BW, et al. Profiles of hemodynamics and oxygen transport derived by using continuous measured oxygen consumption after the Norwood procedure. J Thorac Cardiovasc Surg. 2007. 133:441–448.25. Schranz D, Michel-Behnke I, Akintuerk H. Letter by Schranz et al regarding article, "Comparison of the profiles of postoperative systemic hemodynamics and oxygen transport in neonates after the hybrid or the Norwood procedure: a pilot study". Circulation. 2008. 117:e296. author reply e297-8.26. Honjo O, Benson LN, Mewhort HE, et al. Clinical outcomes, program evolution, and pulmonary artery growth in single ventricle palliation using hybrid and Norwood palliative strategies. Ann Thorac Surg. 2009. 87:1885–1892. discussion 1892-3.27. Kern JH, Hinton VJ, Nereo NE, Hayes CJ, Gersony WM. Early developmental outcome after the Norwood procedure for hypoplastic left heart syndrome. Pediatrics. 1998. 102:1148–1152.28. Mahle WT, Visconti KJ, Freier MC, et al. Relationship of surgical approach to neurodevelopmental outcomes in hypoplastic left heart syndrome. Pediatrics. 2006. 117:e90–e97.29. Licht DJ, Shera DM, Clancy RR, et al. Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg. 2009. 137:529–536. discussion 536-7.30. Miller SP, McQuillen PS, Hamrick S, et al. Abnormal brain development in newborns with congenital heart disease. N Engl J Med. 2007. 357:1928–1938.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 2 Cases of Hypoplastic Left Heart Syndrome
- Biventricular Repair after Bilateral Pulmonary Artery Banding as a Rescue Procedure for a Neonate with Hypoplastic Left Heart Complex
- Hypoplastic Left Heart Syndrome : Report of a Unique Survivor
- A False Diagnosis of Hypoplastic Left Heart Syndrome in a Fetus
- Staged Repair after Hybrid Palliation for Interrupted Aortic Arch with Systemic Outflow Tract Obstruction