J Korean Soc Radiol.
2015 Nov;73(5):307-311. 10.3348/jksr.2015.73.5.307.
Congenital Osteofibrous Dysplasia, Involving the Tibia of a Neonate
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. shlee@amc.seoul.kr
- 2Department of Radiology, Dankook University Hospital, Cheonan, Korea.
- KMID: 2079565
- DOI: http://doi.org/10.3348/jksr.2015.73.5.307
Abstract
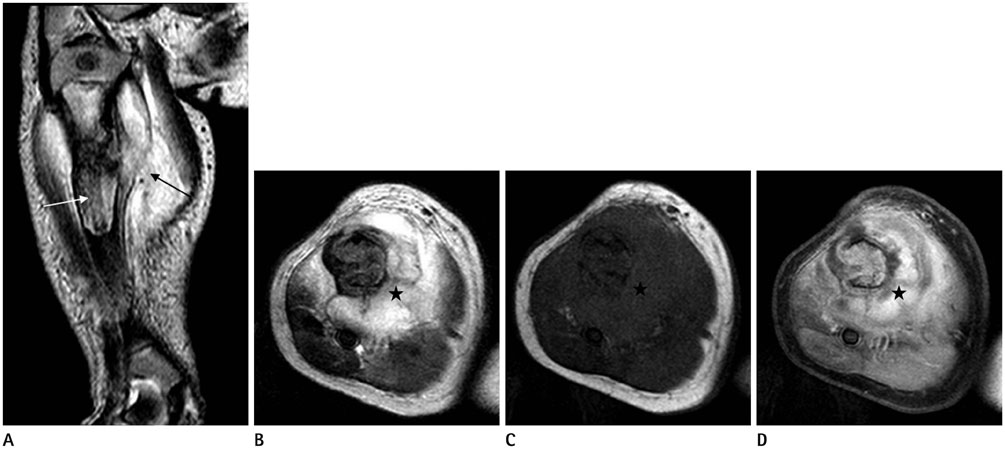
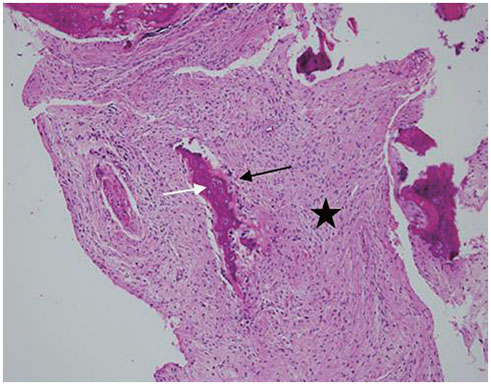
- Osteofibrous dysplasia (OFD) is a benign fibro-osseous lesion found in long bones, and congenital OFD in neonates is very rare. The diagnosis of OFD in neonates is difficult, and it is sometimes misidentified as any of a number of other congenital tumors or tumor-like lesions, in which case biopsies are often necessary. After a histological confirmation of OFD, non-surgical or delayed surgical treatment is generally recommended. We present image findings from the radiographs and magnetic resonance images in the case of a 7-day-old female infant with pathologically confirmed congenital OFD.
Figure
Reference
-
1. Jobke B, Bohndorf K, Vieth V, Werner M. Congenital osteofibrous dysplasia Campanacci: spontaneous postbioptic regression. J Pediatr Hematol Oncol. 2014; 36:249–252.2. Zamzam MM. Congenital osteofibrous dysplasia of the tibia, associated with pseudoarthrosis of the ipsilateral fibula. Saudi Med J. 2008; 29:1507–1509.3. Smith NM, Byard RW, Foster B, Morris L, Clark B, Bourne AJ. Congenital ossifying fibroma (osteofibrous dysplasia) of the tibia--a case report. Pediatr Radiol. 1991; 21:449–451.4. Hahn SB, Kang ES, Jahng JS, Park BM, Choi JC. Ossifying fibroma. Yonsei Med J. 1991; 32:347–355.5. Jung JY, Jee WH, Hong SH, Kang HS, Chung HW, Ryu KN, et al. MR findings of the osteofibrous dysplasia. Korean J Radiol. 2014; 15:114–122.6. Teo HE, Peh WC, Akhilesh M, Tan SB, Ishida T. Congenital osteofibrous dysplasia associated with pseudoarthrosis of the tibia and fibula. Skeletal Radiol. 2007; 36:Suppl 1. S7–S14.7. Stull MA, Kransdorf MJ, Devaney KO. Langerhans cell histiocytosis of bone. Radiographics. 1992; 12:801–823.8. Ang P, Tay YK, Walford NQ. Infantile myofibromatosis: a case report and review of the literature. Cutis. 2004; 73:229–231.9. Maffulli N, Fixsen JA. Pseudoarthrosis of the ulna in neurofibromatosis. A report of four cases. Arch Orthop Trauma Surg. 1991; 110:204–207.10. Kozlowski K, Beluffi G, Cohen DH, Padovani J, Tamaela L, Azouz M, et al. Primary bone tumours in infants. Short literature review and report of 10 cases. Pediatr Radiol. 1985; 15:359–367.