Korean J Pain.
2014 Apr;27(2):178-185. 10.3344/kjp.2014.27.2.178.
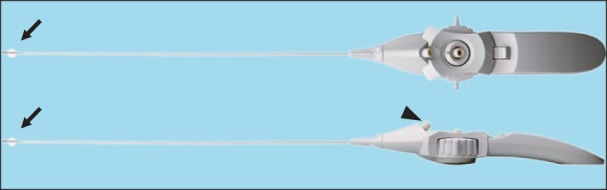
A Novel Balloon-Inflatable Catheter for Percutaneous Epidural Adhesiolysis and Decompression
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sjinwoo@hotmail.com
- KMID: 2074066
- DOI: http://doi.org/10.3344/kjp.2014.27.2.178
Abstract
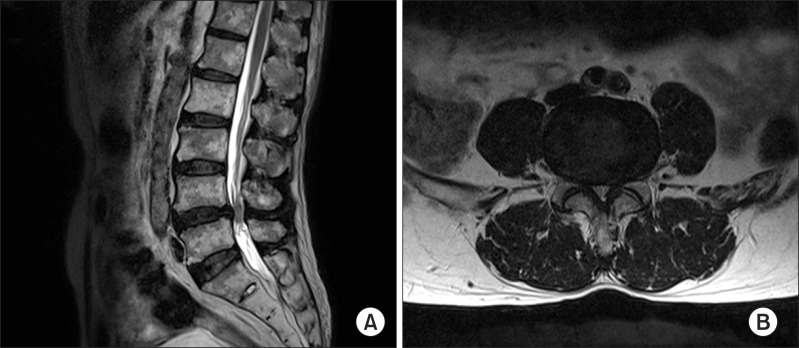
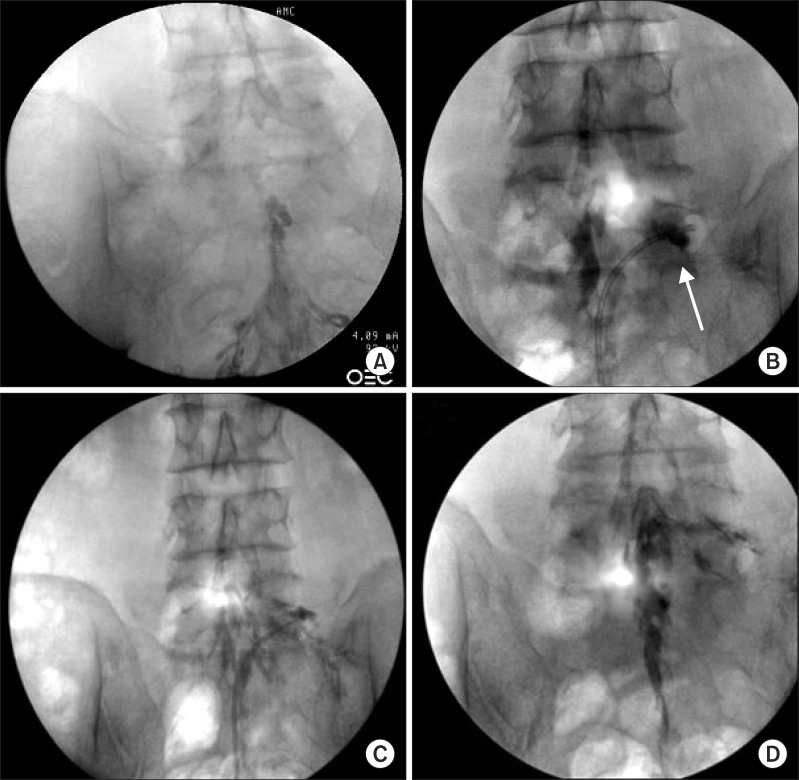
- Epidural adhesions cause pain by interfering with the free movement of the spinal nerves and increasing neural sensitivity as a consequence of neural compression. To remove adhesions and deliver injected drugs to target sites, percutaneous epidural adhesiolysis (PEA) is performed in patients who are unresponsive to conservative treatments. We describe four patients who were treated with a newly developed inflatable balloon catheter for more effective PEA and relief of stenosis. In the present patients, treatments with repetitive epidural steroid injection and/or PEA with the Racz catheter or the NaviCath did not yield long-lasting effects or functional improvements. However, PEA and decompression with the inflatable balloon catheter led to maintenance of pain relief for more than seven months and improvements in the functional status with increases in the walking distance. The present case series suggests that the inflatable balloon catheter may be an effective alternative to performing PEA when conventional methods fail to remove adhesions or sufficiently relieve stenosis.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Lumbar foraminal neuropathy: an update on non-surgical management
Young Kook Choi
Korean J Pain. 2019;32(3):147-159. doi: 10.3344/kjp.2019.32.3.147.Percutaneous epidural balloon neuroplasty: a narrative review of current evidence
Doo-Hwan Kim, Jin-Woo Shin, Seong-Soo Choi
Anesth Pain Med. 2022;17(4):361-370. doi: 10.17085/apm.22237.
Reference
-
1. Berthelot JM, LeGoff B, Maugars Y. The role for radicular veins in nerve root pain is underestimated: limitations of imaging studies. Joint Bone Spine. 2011; 78:115–117. PMID: 21273107.
Article2. Cooper RG, Freemont AJ, Hoyland JA, Jenkins JP, West CG, Illingworth KJ, et al. Herniated intervertebral disc-associated periradicular fibrosis and vascular abnormalities occur without inflammatory cell infiltration. Spine (Phila Pa 1976). 1995; 20:591–598. PMID: 7604329.
Article3. Kobayashi S, Baba H, Uchida K, Kokubo Y, Kubota C, Yamada S, et al. Effect of mechanical compression on the lumbar nerve root: localization and changes of intraradicular inflammatory cytokines, nitric oxide, and cyclooxygenase. Spine (Phila Pa 1976). 2005; 30:1699–1705. PMID: 16094269.
Article4. Anderson SR, Racz GB, Heavner J. Evolution of epidural lysis of adhesions. Pain Physician. 2000; 3:262–270. PMID: 16906184.
Article5. Armon C, Argoff CE, Samuels J, Backonja MM. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007; 68:723–729. PMID: 17339579.
Article6. Hong JH, Lee YC, Lee HM, Kang CH. An analysis of the outcome of transforaminal epidural steroid injections in patients with spinal stenosis or herniated intervertebral discs. Korean J Pain. 2008; 21:38–43.
Article7. Manchikanti L, Bakhit CE. Percutaneous lysis of epidural adhesions. Pain Physician. 2000; 3:46–64. PMID: 16906207.
Article8. Manchikanti L, Singh V, Bakhit CE, Fellows B. Interventional techniques in the management of chronic pain: part 1.0. Pain Physician. 2000; 3:7–42. PMID: 16906205.9. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis using Navicath for the management of chronic pain due to lumbosacral disc herniation. Pain Physician. 2012; 15:213–221. PMID: 22622905.10. Birkenmaier C, Baumert S, Schroeder C, Jansson V, Wegener B. A biomechanical evaluation of the epidural neurolysis procedure. Pain Physician. 2012; 15:E89–E97. PMID: 22270752.11. Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013; 16:S49–S283. PMID: 23615883.12. Kim SH, Choi WJ, Suh JH, Jeon SR, Hwang CJ, Koh WU, et al. Effects of transforaminal balloon treatment in patients with lumbar foraminal stenosis: a randomized, controlled, double-blind trial. Pain Physician. 2013; 16:213–224. PMID: 23703408.13. Massie JB, Huang B, Malkmus S, Yaksh TL, Kim CW, Garfin SR, et al. A preclinical post laminectomy rat model mimics the human post laminectomy syndrome. J Neurosci Methods. 2004; 137:283–289. PMID: 15262072.
Article14. Haq I, Cruz-Almeida Y, Siqueira EB, Norenberg M, Green BA, Levi AD. Postoperative fibrosis after surgical treatment of the porcine spinal cord: a comparison of dural substitutes. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2005; 2:50–54. PMID: 15658126.
Article15. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 1999; 24:202–207. PMID: 10338168.
Article16. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–E462. PMID: 22828693.17. Helm S, Hayek SM, Colson J, Chopra P, Deer TR, Justiz R, et al. Spinal endoscopic adhesiolysis in post lumbar surgery syndrome: an update of assessment of the evidence. Pain Physician. 2013; 16:SE125–SE150. PMID: 23615889.18. Kim JD, Jang JH, Jung GH, Kim JY, Jang SJ. Epiduroscopic laser disc and neural decompression. J Neurosurg Rev [serial on the Internet]. 2012. 3. 2012 Mar 22. Available at http://neurosurgicalreview.com/2012/03/epiduroscopic/.19. Song SO, Lim HJ. Clinical experience of epidural adhesiolysis in patients with failed back surgery syndrome. Korean J Anesthesiol. 2004; 47:547–552.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful electrode insertion for spinal cord stimulation after balloon adhesiolysis in a patient with epidural adhesion - A case report -
- Clinical Experience of Epidural Adhesiolysis in Patients with Failed Back Surgery Syndrome
- Percutaneous Drainage of Epidural abscess in Lumbar Spin: Case Report
- Percutaneous Epidural Neuroplasty
- Percutaneous epidural balloon neuroplasty: a narrative review of current evidence