Korean J Pain.
2011 Jun;24(2):93-99. 10.3344/kjp.2011.24.2.93.
Piriformis Syndrome in Knee Osteoarthritis Patients after Wearing Rocker Bottom Shoes
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- KMID: 2074004
- DOI: http://doi.org/10.3344/kjp.2011.24.2.93
Abstract
- BACKGROUND
Rocker bottom shoes (RBS) are popular among patients with different foot, leg, or back problems in Korea. Patients with knee osteoarthritis concurrent weakness in the quadriceps femoris muscle, who wear these shoes, are often assumed to develop piriformis syndrome (PS). This study was performed to improve the understanding about the effect of wearing such shoes on duration of the syndrome in knee osteoarthritis.
METHODS
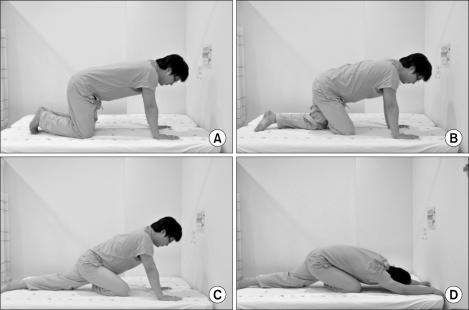
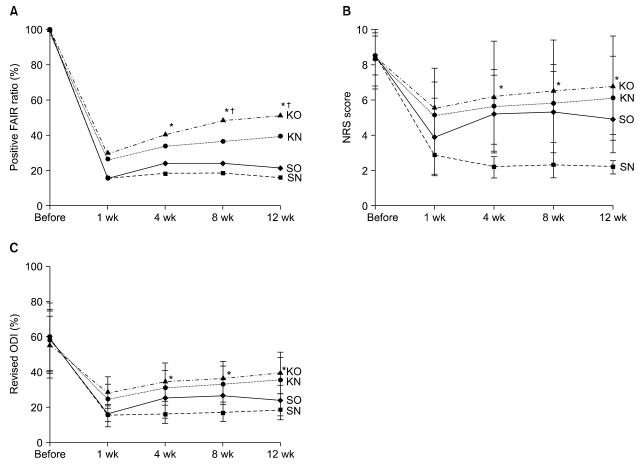
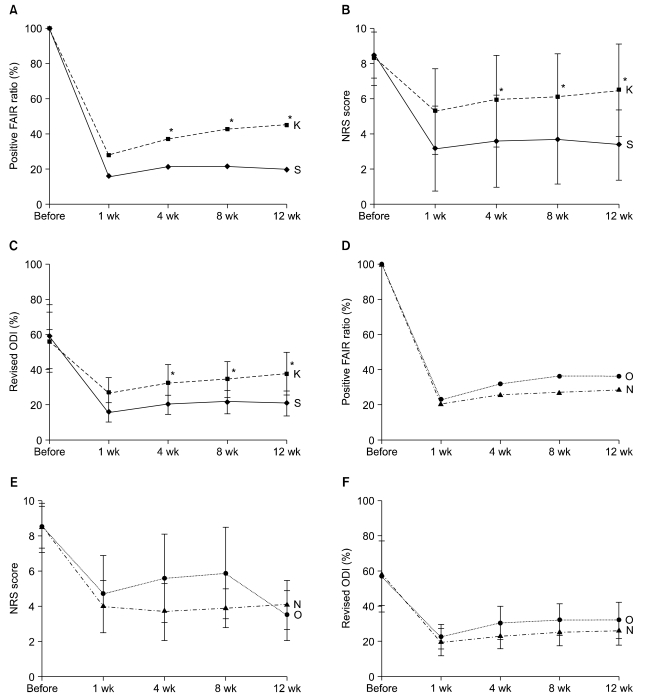
We randomly assigned 150 patients with PS, who had used RBS daily for at least 6 months, to 2 groups, the S (stopped wearing) and K (kept wearing) groups. Both the groups were subdivided into the O and N groups, comprising patients with and without knee osteoarthritis, respectively. The effects of the treatment, including piriformis muscle injections and a home exercise program, were compared between the 2 groups by using a flexion-adduction-internal rotation (FAIR) test, a numeric rating scale (NRS), and the revised Oswestry disability index (ODI) during the 12-week follow-up.
RESULTS
The positive FAIR test ratios, mean NRS scores, and revised ODIs were higher in the KO group than the SN group from 4?12 weeks after treatment.
CONCLUSIONS
RBS may extend duration of the PS in osteoarthritis patients.
MeSH Terms
Figure
Cited by 1 articles
-
Interventional Pain Management in Rheumatological Diseases - A Three Years Physiatric Experience in a Tertiary Medical College Hospital in Bangladesh
Md Abu Bakar Siddiq, Suzon Al Hasan, Gautam Das, Amin Uddin A Khan
Korean J Pain. 2011;24(4):205-215. doi: 10.3344/kjp.2011.24.4.205.
Reference
-
1. Romkes J, Rudmann C, Brunner R. Changes in gait and EMG when walking with the masai barefoot technique. Clin Biomech (Bristol, Avon). 2006; 21:75–81.
Article2. Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009; 40:10–18. PMID: 19466717.
Article3. Dere K, Akbas M, Luleci N. A rare cause of a piriformis syndrome. J Back Musculoskelet Rehabil. 2009; 22:55–58. PMID: 20023365.
Article4. Messier SP, Loeser RF, Hoover JL, Semble EL, Wise CM. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehabil. 1992; 73:29–36. PMID: 1729969.5. Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997; 127:97–104. PMID: 9230035.
Article6. Lewek MD, Rudolph KS, Snyder-Mackler L. Quadriceps femoris muscle weakness and activation failure in patients with symptomatic knee osteoarthritis. J Orthop Res. 2004; 22:110–115. PMID: 14656668.
Article7. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957; 16:494–502. PMID: 13498604.
Article8. Fairbank JC, Pynsent PB. The oswestry disability index. Spine. 2000; 25:2940–2952. PMID: 11074683.
Article9. Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002; 82:8–24. PMID: 11784274.
Article10. Ross LM, Lamperti ED. Thieme atlas of anatomy: General anatomy and musculoskeletal system. 2006. Stuttgart: Thieme;p. 360–509.11. Albright BC, Woodhull-Smith WM. Rocker bottom soles alter the postural response to backward translation during stance. Gait Posture. 2009; 30:45–49. PMID: 19329317.
Article12. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976; 124:435–439. PMID: 132772.13. Jenkyn TR, Hunt MA, Jones IC, Giffin JR, Birmingham TB. Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism. J Biomech. 2008; 41:276–283. PMID: 18061197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plantar Pressure Reducing Effect of Diabetic Shoes with Different Rigid Rockers
- Looking beyond Piriformis Syndrome: Is It Really the Piriformis?
- The Effect of Laterally Wedged Insoles on Standing Balance of Patients with Osteoarthritis in the Medial Compartment of Knees
- Post-radiation Piriformis Syndrome in a Cervical Cancer Patient: A Case Report
- The Effects of Subtalar Joint Ankle Brace and Shoes on Static Postural Balance in Elderly