Yonsei Med J.
2015 Mar;56(2):348-354. 10.3349/ymj.2015.56.2.348.
Risk Factors for Mortality in Patients with Serratia marcescens Bacteremia
- Affiliations
-
- 1Division of Infectious Disease, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. smileboy9@yuhs.ac
- 2AIDS Research Institute, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2070009
- DOI: http://doi.org/10.3349/ymj.2015.56.2.348
Abstract
- PURPOSE
Over the last 30 years, Serratia marcescens (S. marcescens) has emerged as an important pathogen, and a common cause of nosocomial infections. The aim of this study was to identify risk factors associated with mortality in patients with S. marcescens bacteremia.
MATERIALS AND METHODS
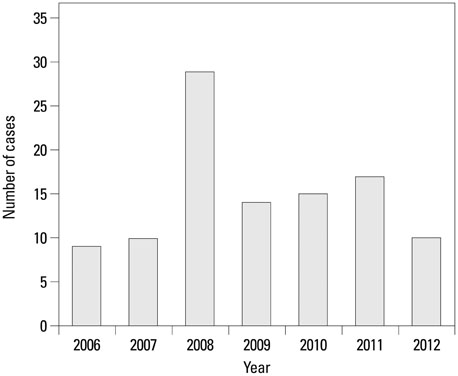
We performed a retrospective cohort study of 98 patients who had one or more blood cultures positive for S. marcescens between January 2006 and December 2012 in a tertiary care hospital in Seoul, South Korea. Multiple risk factors were compared with association with 28-day all-cause mortality.
RESULTS
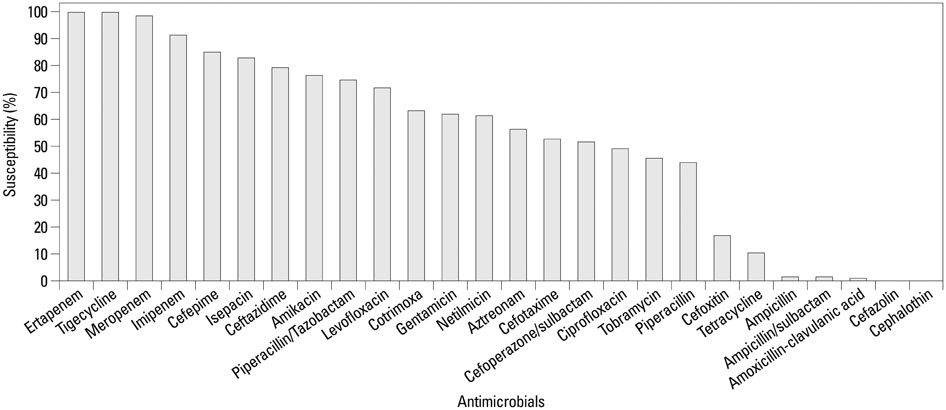
The 28-day mortality was 22.4% (22/98 episodes). In a univariate analysis, the onset of bacteremia during the intensive care unit stay (p=0.020), serum albumin level (p=0.011), serum C-reactive protein level (p=0.041), presence of indwelling urinary catheter (p=0.023), and Sequential Oran Failure Assessment (SOFA) score at the onset of bacteremia (p<0.001) were significantly different between patients in the fatal and non-fatal groups. In a multivariate analysis, lower serum albumin level and an elevated SOFA score were independently associated with 28-day mortality [adjusted odds ratio (OR) 0.206, 95% confidential interval (CI) 0.044-0.960, p=0.040, and adjusted OR 1.474, 95% CI 1.200-1.810, p<0.001, respectively].
CONCLUSION
Lower serum albumin level and an elevated SOFA score were significantly associated with adverse outcomes in patients with S. marcescens bacteremia.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Anti-Bacterial Agents/therapeutic use
Bacteremia/drug therapy/microbiology/*mortality
Cross Infection/mortality
Female
Humans
Intensive Care Units
Male
Middle Aged
Multiple Organ Failure
Republic of Korea/epidemiology
Retrospective Studies
Risk Factors
Serratia Infections/diagnosis/drug therapy/*mortality
Serratia marcescens/drug effects/*isolation & purification
Severity of Illness Index
Survival Rate
Time Factors
Treatment Outcome
Anti-Bacterial Agents
Figure
Reference
-
1. Eisenstein BI, Zaleznik DF. Enterobacteriaceae. In : Mandell GL, Douglas RG, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 5th ed. Philadelphia: Churchill Livingstone;2000. p. 2297–2310.2. Yu VL. Serratia marcescens: historical perspective and clinical review. N Engl J Med. 1979; 300:887–893.3. Henjyoji EY, Whitson TC, Oashi DK, Allen BD. Bacteremia due to Serratia marcescens. J Trauma. 1971; 11:417–421.
Article4. Luzzaro F, Perilli M, Migliavacca R, Lombardi G, Micheletti P, Agodi A, et al. Repeated epidemics caused by extended-spectrum beta-lactamase-producing Serratia marcescens strains. Eur J Clin Microbiol Infect Dis. 1998; 17:629–636.
Article5. Bonnet R, Sampaio JL, Chanal C, Sirot D, De Champs C, Viallard JL, et al. A novel class A extended-spectrum beta-lactamase (BES-1) in Serratia marcescens isolated in Brazil. Antimicrob Agents Chemother. 2000; 44:3061–3068.
Article6. Ivanova D, Markovska R, Hadjieva N, Schneider I, Mitov I, Bauernfeind A. Extended-spectrum beta-lactamase-producing Serratia marcescens outbreak in a Bulgarian hospital. J Hosp Infect. 2008; 70:60–65.
Article7. Saito H, Elting L, Bodey GP, Berkey P. Serratia bacteremia: review of 118 cases. Rev Infect Dis. 1989; 11:912–920.
Article8. Wong WW, Wang LS, Cheng DL, Lin SJ, Chin TD, Hinthorn DR, et al. Serratia marcescens bacteremia. J Formos Med Assoc. 1991; 90:88–93.9. Yu WL, Lin CW, Wang DY. Serratia marcescens bacteremia: clinical features and antimicrobial susceptibilities of the isolates. J Microbiol Immunol Infect. 1998; 31:171–179.10. Shih HI, Lee HC, Lee NY, Chang CM, Wu CJ, Wang LR, et al. Serratia marcescens bacteremia at a medical center in southern Taiwan: high prevalence of cefotaxime resistance. J Microbiol Immunol Infect. 2005; 38:350–357.11. Cheong HS, Ko KS, Kang CI, Chung DR, Peck KR, Song JH. Clinical significance of infections caused by extended-spectrum β-lactamase-producing Enterobacteriaceae blood isolates with inducible AmpC β-lactamase. Microb Drug Resist. 2012; 18:446–452.
Article12. Choi SH, Kim YS, Chung JW, Kim TH, Choo EJ, Kim MN, et al. Serratia bacteremia in a large university hospital: trends in antibiotic resistance during 10 years and implications for antibiotic use. Infect Control Hosp Epidemiol. 2002; 23:740–747.
Article13. Engel HJ, Collignon PJ, Whiting PT, Kennedy KJ. Serratia sp. bacteremia in Canberra, Australia: a population-based study over 10 years. Eur J Clin Microbiol Infect Dis. 2009; 28:821–824.
Article14. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26:1793–1800.
Article15. Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Oh MD, et al. Bloodstream infections caused by Enterobacter species: predictors of 30-day mortality rate and impact of broad-spectrum cephalosporin resistance on outcome. Clin Infect Dis. 2004; 39:812–818.
Article16. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002; 137:791–797.
Article17. Marik PE, Lipman J. The definition of septic shock: implications for treatment. Crit Care Resusc. 2007; 9:101–103.18. World Health Organization. International statistical classification of diseases and related health problems. 10th revision. 2nd ed. Geneva: World Health Organization;2004.19. Harbarth S, Garbino J, Pugin J, Romand JA, Lew D, Pittet D. Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med. 2003; 115:529–535.
Article20. McGregor JC, Rich SE, Harris AD, Perencevich EN, Osih R, Lodise TP Jr, et al. A systematic review of the methods used to assess the association between appropriate antibiotic therapy and mortality in bacteremic patients. Clin Infect Dis. 2007; 45:329–337.
Article21. Song SW, Kim KT, Ku YM, Park SH, Kim YS, Lee DG, et al. Clinical role of interstitial pneumonia in patients with scrub typhus: a possible marker of disease severity. J Korean Med Sci. 2004; 19:668–673.
Article22. Carratalà J, Rosón B, Fernández-Sabé N, Shaw E, del Rio O, Rivera A, et al. Factors associated with complications and mortality in adult patients hospitalized for infectious cellulitis. Eur J Clin Microbiol Infect Dis. 2003; 22:151–157.
Article23. Clinical and Laboratory Standards Institue. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Second Informational Supplement M100-S21. Wayne, PA, USA: CLSI;2012.24. Haddy RI, Mann BL, Nadkarni DD, Cruz RF, Elshoff DJ, Buendia FC, et al. Nosocomial infection in the community hospital: severe infection due to Serratia species. J Fam Pract. 1996; 42:273–277.25. Laupland KB, Parkins MD, Gregson DB, Church DL, Ross T, Pitout JD. Population-based laboratory surveillance for Serratia species isolates in a large Canadian health region. Eur J Clin Microbiol Infect Dis. 2008; 27:89–95.
Article26. Park YJ, Park SY, Oh EJ, Park JJ, Lee KY, Woo GJ, et al. Occurrence of extended-spectrum beta-lactamases among chromosomal AmpC-producing Enterobacter cloacae, Citrobacter freundii, and Serratia marcescens in Korea and investigation of screening criteria. Diagn Microbiol Infect Dis. 2005; 51:265–269.
Article27. Nordmann P, Naas T, Poirel L. Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011; 17:1791–1798.28. Kim SY, Shin J, Shin SY, Ko KS. Characteristics of carbapenem-resistant Enterobacteriaceae isolates from Korea. Diagn Microbiol Infect Dis. 2013; 76:486–490.
Article29. Arribas JR, Dominguez A, Folgueira MD, Peña P, Luengo S, Peña JM, et al. Prognostic factors in Serratia bacteremia. Rev Infect Dis. 1990; 12:563–564.
Article30. Ho PL, Shek RH, Chow KH, Duan RS, Mak GC, Lai EL, et al. Detection and characterization of extended-spectrum beta-lactamases among bloodstream isolates of Enterobacter spp. in Hong Kong, 2000-2002. J Antimicrob Chemother. 2005; 55:326–332.
Article31. Watanakunakorn C. Serratia bacteremia: a review of 44 episodes. Scand J Infect Dis. 1989; 21:477–483.
Article32. Herrmann FR, Safran C, Levkoff SE, Minaker KL. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch Intern Med. 1992; 152:125–130.
Article33. Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003; 237:319–334.34. Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J. The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet. 2011; 50:99–110.
Article35. Routsi C, Pratikaki M, Sotiropoulou C, Platsouka E, Markaki V, Paniara O, et al. Application of the sequential organ failure assessment (SOFA) score to bacteremic ICU patients. Infection. 2007; 35:240–244.
Article36. Anami EH, Grion CM, Cardoso LT, Kauss IA, Thomazini MC, Zampa HB, et al. Serial evaluation of SOFA score in a Brazilian teaching hospital. Intensive Crit Care Nurs. 2010; 26:75–82.
Article37. Ku NS, Han SH, Kim CO, Baek JH, Jeong SJ, Jin SJ, et al. Risk factors for mortality in patients with Burkholderia cepacia complex bacteraemia. Scand J Infect Dis. 2011; 43:792–797.
Article38. Kim BN, Lee SO, Choi SH, Kim NJ, Woo JH, Ryu J, et al. Outcome of antibiotic therapy for third-generation cephalosporin-resistant Gram-negative bacteraemia: an analysis of 249 cases caused by Citrobacter, Enterobacter and Serratia species. Int J Antimicrob Agents. 2003; 22:106–111.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep Cutaneous Ulcer Caused by Serratia marcescens after Fresh Water Exposure
- Serratia Marcescens Keratitis
- A Case of Cellulitis Caused by Serratia marcescens in a Patient with Acute Lymphocytic Leukemia
- Skin Infection Caused by Serratia marcescens in an Immunocompetent Patient with Hidradenitis Suppurativa
- Clinical Bacteriologic Study of Serratia Marcescens Septicemia