J Korean Med Sci.
2014 Dec;29(12):1678-1683. 10.3346/jkms.2014.29.12.1678.
Surgeon Custom-Made Iliac Branch Device to Salvage Hypogastric Artery during Endovascular Aneurysm Repair
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Daegu Catholic University College of Medicine, Daegu, Korea. khpark@cu.ac.kr
- 2Department of Surgery, Yeungnam University, College of Medicine, Daegu, Korea.
- KMID: 2069958
- DOI: http://doi.org/10.3346/jkms.2014.29.12.1678
Abstract
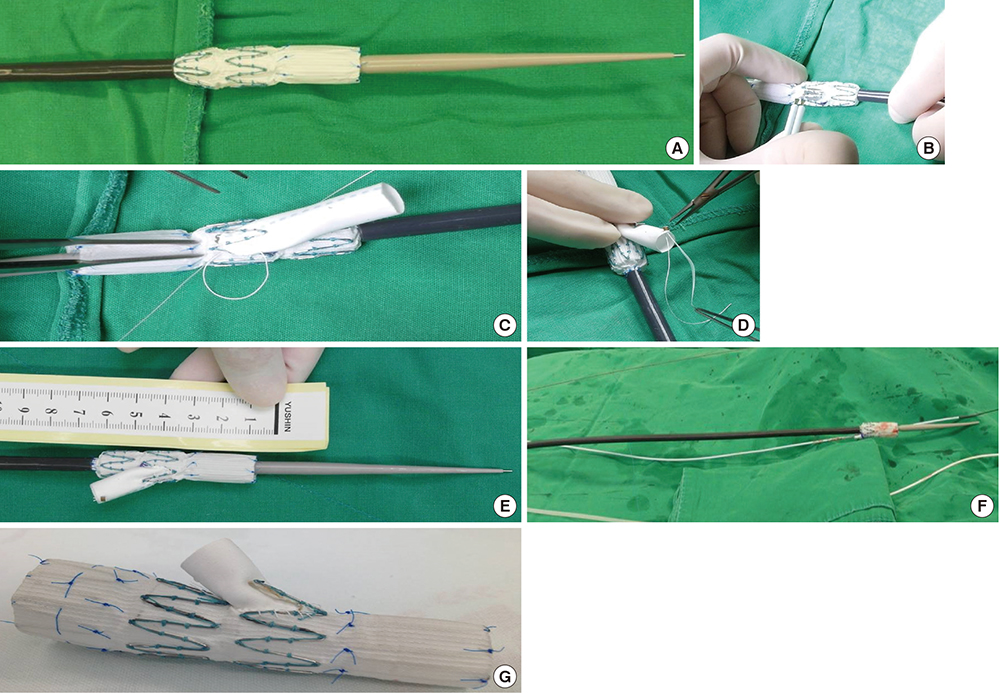
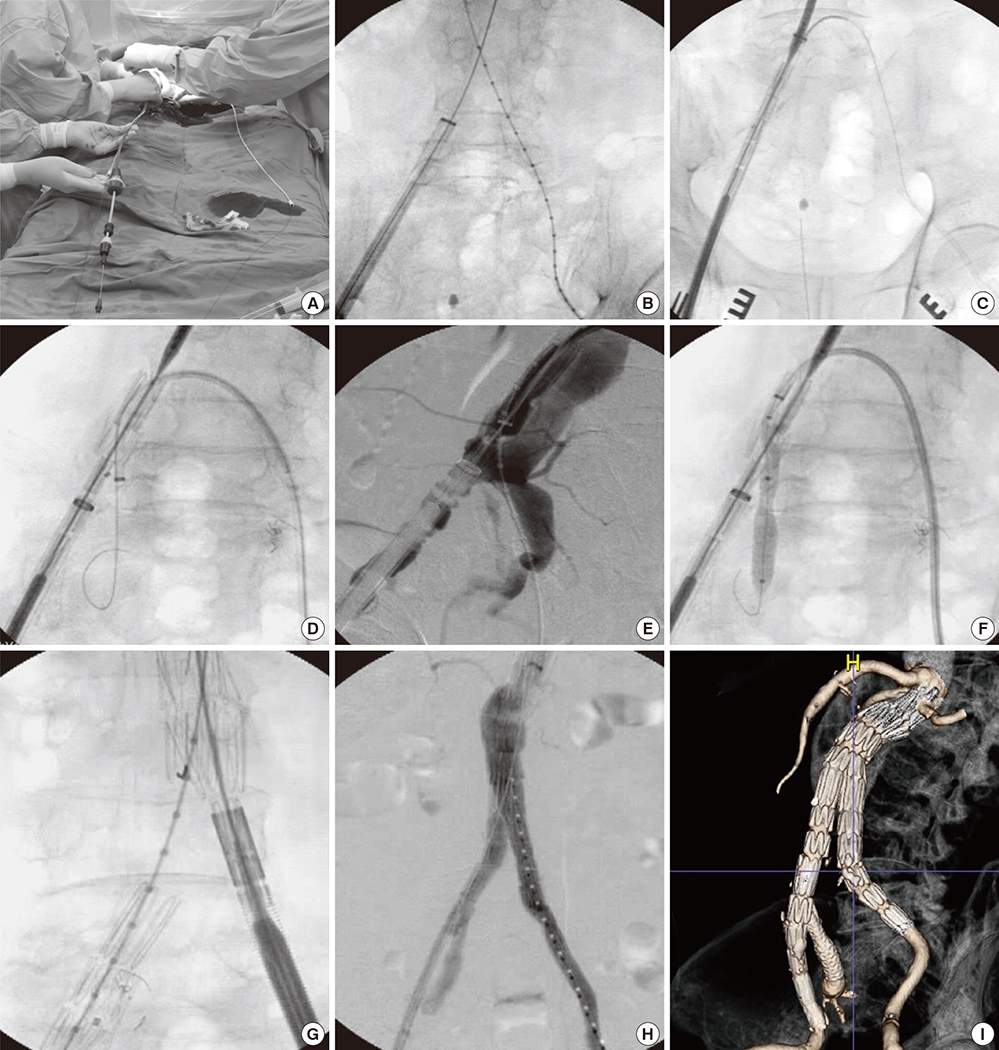
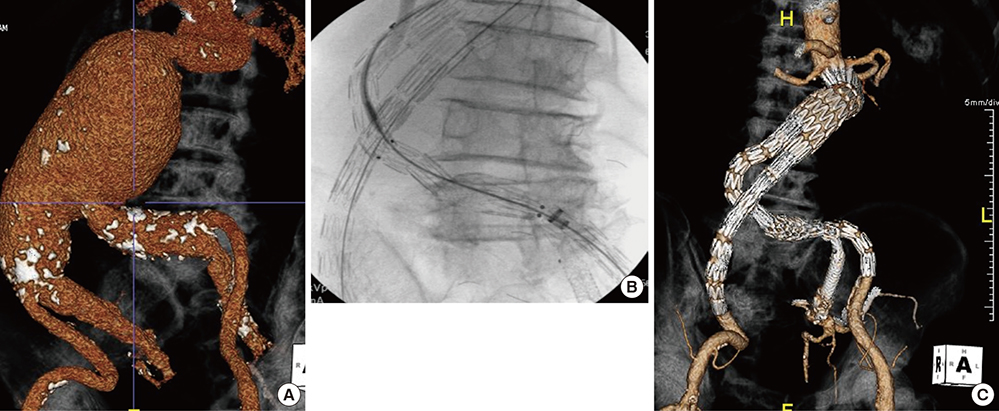
- Endovascular salvage of the hypogastric artery using iliac branch device (IBD) during endovascular aortic aneurysm repair (EVAR), offers less invasive alternative solution to surgery to prevent pelvic ischemia. We have performed the first Korean surgeon custom-made IBD for this purpose to overcome the limitation of unavailability of the devices in Korea. Four patients with abdominal aortic aneurysm with bilateral common iliac artery aneurysm (CIAA) were treated using custom-made IBDs from October 2013 to December 2013. IBD was created in back table before EVAR operation using TFLE Zenith iliac limb stent graft (Cook Inc.). Three V12 (Atrium, Inc.) one Viabahn (Gore, Inc.) were used for bridging between IBD and target hypogastric artery. With this modification of IBD procedure, exteriorize the guide wire without snare device is possible which offers another benefit in terms of reducing medical costs comparing to commercial IBD. All operations were successful without any device related complications or postoperative endoleaks. During the mean follow up of 3 months, all IBD were patent without clinical complications. Surgeon custom made IBD is feasible and useful to preserve pelvic perfusion especially in the situation of limited commercial IBD availability in many countries. Long-term follow-up is needed to evaluate stent graft patency and IBD-related complications.
MeSH Terms
Figure
Reference
-
1. Aburahma AF, Campbell JE, Mousa AY, Hass SM, Stone PA, Jain A, Nanjundappa A, Dean LS, Keiffer T, Habib J. Clinical outcomes for hostile versus favorable aortic neck anatomy in endovascular aortic aneurysm repair using modular devices. J Vasc Surg. 2011; 54:13–21.2. Stather PW, Sayers RD, Cheah A, Wild JB, Bown MJ, Choke E. Outcomes of endovascular aneurysm repair in patients with hostile neck anatomy. Eur J Vasc Endovasc Surg. 2012; 44:556–561.3. Early H, Atkins M. Technical tips for managing difficult iliac access. Semin Vasc Surg. 2012; 25:138–143.4. Armon MP, Wenham PW, Whitaker SC, Gregson RH, Hopkinson BR. Common iliac artery aneurysms in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 1998; 15:255–257.5. Connolly JE, Ingegno M, Wilson SE. Preservation of the pelvic circulation during infrarenal aortic surgery. Cardiovasc Surg. 1996; 4:65–70.6. Lee CW, Kaufman JA, Fan CM, Geller SC, Brewster DC, Cambria RP, Lamuraglia GM, Gertler JP, Abbott WM, Waltman AC. Clinical outcome of internal iliac artery occlusions during endovascular treatment of aortoiliac aneurysmal diseases. J Vasc Interv Radiol. 2000; 11:567–571.7. Lin PH, Bush RL, Chaikof EL, Chen C, Conklin B, Terramani TT, Brinkman WT, Lumsden AB. A prospective evaluation of hypogastric artery embolization in endovascular aortoiliac aneurysm repair. J Vasc Surg. 2002; 36:500–506.8. Lin PH, Chen AY, Vij A. Hypogastric artery preservation during endovascular aortic aneurysm repair: is it important? Semin Vasc Surg. 2009; 22:193–200.9. Arko FR, Lee WA, Hill BB, Fogarty TJ, Zarins CK. Hypogastric artery bypass to preserve pelvic circulation: improved outcome after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2004; 39:404–408.10. Parlani G, Verzini F, De Rango P, Brambilla D, Coscarella C, Ferrer C, Cao P. Long-term results of iliac aneurysm repair with iliac branched endograft: a 5-year experience on 100 consecutive cases. Eur J Vasc Endovasc Surg. 2012; 43:287–292.11. Ferreira M, Monteiro M, Lanziotti L. Technical aspects and midterm patency of iliac branched devices. J Vasc Surg. 2010; 51:545–550. discussion 50.12. Oderich GS, Ricotta JJ 2nd. Novel surgeon-modified hypogastric branch stent graft to preserve pelvic perfusion. Ann Vasc Surg. 2010; 24:278–286.13. Parodi JC, Barone A, Piraino R, Schonholz C. Endovascular treatment of abdominal aortic aneurysms: lessons learned. J Endovasc Surg. 1997; 4:102–110.14. Ghosh J, Murray D, Paravastu S, Farquharson F, Walker MG, Serracino-Inglott F. Contemporary management of aorto-iliac aneurysms in the endovascular era. Eur J Vasc Endovasc Surg. 2009; 37:182–188.15. Friedman SG, Wun H. Hypogastric preservation with Viabahn stent graft during endovascular aneurysm repair. J Vasc Surg. 2011; 54:504–506.16. Oderich GS, Ricotta JJ 2nd. Modified fenestrated stent grafts: device design, modifications, implantation, and current applications. Perspect Vasc Surg Endovasc Ther. 2009; 21:157–167.17. Ricotta JJ 2nd, Tsilimparis N. Surgeon-modified fenestrated-branched stent grafts to treat emergently ruptured and symptomatic complex aortic aneurysms in high-risk patients. J Vasc Surg. 2012; 56:1535–1542.18. Starnes BW. Physician-modified endovascular grafts for the treatment of elective, symptomatic, or ruptured juxtarenal aortic aneurysms. J Vasc Surg. 2012; 56:601–607.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- EVAR with Hypogastric Artery Bypass in Patient with Abdominal Aorto-Iliac Aneurysm
- Endovascular Repair of Thoracic Aortic Aneurysm Using a Custom-made Fenestrated Stent Graft to Preserve the Left Subclavian Artery
- Novel Strategies for the Hostile Iliac Artery during Endovascular Aortic Aneurysm Repair
- Endovascular aortic aneurysm repair using a bifurcated stent graft in a patient with femoro-femoral bypass
- Endovascular Treatment of Isolated Bilateral Common Iliac Artery Aneurysms Using Iliac Branched Stent Graft