J Korean Med Sci.
2014 Nov;29(11):1572-1576. 10.3346/jkms.2014.29.11.1572.
Prevention of Venous Thromboembolism in Medical Intensive Care Unit: A Multicenter Observational Study in Korea
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. cgyoo@snu.ac.kr
- 2Department of Pulmonology, The Catholic University of Korea School of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, University of Dongguk College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 5Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 6Department of Respiratory Medicine and Allergy, Soonchunhyang University School of Medicine, Seoul, Korea.
- 7Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 8Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 9Department of Pulmonary and Critical Care Medicine, Ajou University School of Medicine, Suwon, Korea.
- 10Department of Internal Medicine, College of Medicine, Wonkwang University, Iksan, Korea.
- 11Department of Internal Medicine, College of Medicine, Inha University, Incheon, Korea.
- 12Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2069941
- DOI: http://doi.org/10.3346/jkms.2014.29.11.1572
Abstract
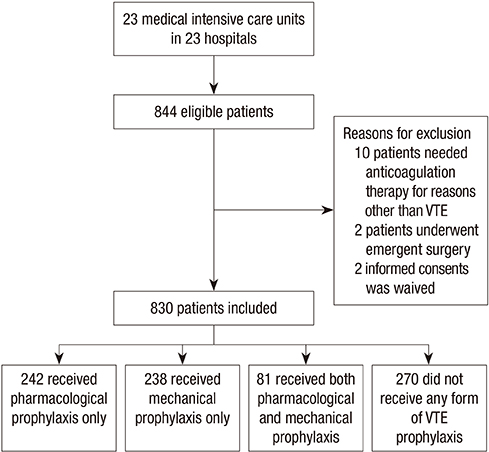
- Patients admitted to medical intensive care unit (MICU) are at increased risk for venous thromboembolism (VTE); and prophylaxis is recommended. However, the actual range and frequency of VTE prophylaxis administered to MICU patients are not well defined. Patients over 40 yr of age and expected MICU stay of more than 48 hr were eligible for this observational cohort study of 23 MICUs in Korea. Patients already on anticoagulation therapy or those requiring anticoagulation for reasons other than VTE were excluded. Among 830 patients, VTE prophylaxis was given to 560 (67.5%) patients. Among 560 patients, 323 (38.9%) received pharmacoprophylaxis, 318 (38.4%) received mechanical prophylaxis and 81 (9.8%) received both forms of prophylaxis. About 74% of patients in the pharmacoprophylaxis group received low molecular weight heparin and 53% of the patients in the mechanical prophylaxis group used intermittent pneumatic compression. Most of the patients (90%) had more than one risk factor for VTE and the most common risk factor was old age, followed by heart and respiratory failure. In this observational cohort study of 23 MICUs in Korea, 67.5% of patients received thromboprophylaxis. Further studies are needed to clarify the role and efficacy of VTE prophylaxis in Korean critically ill patients.
MeSH Terms
-
Adult
Age Factors
Aged
Cohort Studies
Female
Heart Failure/complications
Heparin, Low-Molecular-Weight/therapeutic use
Humans
*Intensive Care Units
Length of Stay
Male
Mechanical Thrombolysis
Middle Aged
Republic of Korea
Respiratory Insufficiency/complications
Retrospective Studies
Risk Factors
Tomography, X-Ray Computed
Venous Thromboembolism/complications/*prevention & control/therapy
Heparin, Low-Molecular-Weight
Figure
Reference
-
1. Davidson BL. Risk assessment and prophylaxis of venous thromboembolism in acutely and/or critically ill patients. Haemostasis. 2000; 30:77–81. discussion 63.2. Cushman M. Epidemiology and risk factors for venous thrombosis. Semin Hematol. 2007; 44:62–69.3. Williams MT, Aravindan N, Wallace MJ, Riedel BJ, Shaw AD. Venous thromboembolism in the intensive care unit. Crit Care Clin. 2003; 19:185–207.4. Attia J, Ray JG, Cook DJ, Douketis J, Ginsberg JS, Geerts WH. Deep vein thrombosis and its prevention in critically ill adults. Arch Intern Med. 2001; 161:1268–1279.5. Patel R, Cook DJ, Meade MO, Griffith LE, Mehta G, Rocker GM, Marshall JC, Hodder R, Martin CM, Heyland DK, et al. Burden of illness in venous thromboembolism in critical care: a multicenter observational study. J Crit Care. 2005; 20:341–347.6. Hirsch DR, Ingenito EP, Goldhaber SZ. Prevalence of deep venous thrombosis among patients in medical intensive care. JAMA. 1995; 274:335–337.7. Marik PE, Andrews L, Maini B. The incidence of deep venous thrombosis in ICU patients. Chest. 1997; 111:661–664.8. Xu XF, Yang YH, Zhai ZG, Liu S, Zhu GF, Li CS, Wang C. Prevalence and incidence of deep venous thrombosis among patients in medical intensive care unit. Zhonghua Liu Xing Bing Xue Za Zhi. 2008; 29:1034–1037.9. Aniwan S, Rojnuckarin P. High incidence of symptomatic venous thromboembolism in Thai hospitalized medical patients without thromboprophylaxis. Blood Coagul Fibrinolysis. 2010; 21:334–338.10. Do JG, Kim DH, Sung DH. Incidence of deep vein thrombosis after spinal cord injury in Korean patients at acute rehabilitation unit. J Korean Med Sci. 2013; 28:1382–1387.11. Twigg SJ, McCrirrick A, Sanderson PM. A comparison of post mortem findings with post hoc estimated clinical diagnoses of patients who die in a United Kingdom intensive care unit. Intensive Care Med. 2001; 27:706–710.12. Geerts W, Cook D, Selby R, Etchells E. Venous thromboembolism and its prevention in critical care. J Crit Care. 2002; 17:95–104.13. Liew NC, Chang YH, Choi G, Chu PH, Gao X, Gibbs H, Ho CO, Ibrahim H, Kim TK, Kritpracha B, et al. Asian venous thromboembolism guidelines: prevention of venous thromboembolism. Int Angiol. 2012; 31:501–516.14. Geerts W, Selby R. Prevention of venous thromboembolism in the ICU. Chest. 2003; 124:357s–363s.15. Chan CM, Shorr AF. Economic and outcomes aspects of venous thromboembolic disease. Crit Care Clin. 2012; 28:113–123. vii16. Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, Cook DJ, Balekian AA, Klein RC, Le H, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: american college of chest physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e195S–e226S.17. Keane MG, Ingenito EP, Goldhaber SZ. Utilization of venous thromboembolism prophylaxis in the medical intensive care unit. Chest. 1994; 106:13–14.18. Parikh KC, Oh D, Sittipunt C, Kalim H, Ullah S, Aggarwal SK. VOICE Asia Investigators. Venous thromboembolism prophylaxis in medical ICU patients in Asia (VOICE Asia): a multicenter, observational, cross-sectional study. Thromb Res. 2012; 129:e152–e158.19. Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9:85–91.20. Bang SM, Jang MJ, Kim KH, Yhim HY, Kim YK, Nam SH, Hwang HG, Bae SH, Kim SH, Mun YC, et al. Prevention of venous thromboembolism, 2nd edition: korean society of thrombosis and hemostasis evidence-based clinical practice guidelines. J Korean Med Sci. 2014; 29:164–171.21. Bang SM, Jang MJ, Oh D, Kim YK, Kim IH, Yoon SS, Yoon HJ, Kim CS, Park S. Korean Society of Thrombosis and Hemostasis. Korean guidelines for the prevention of venous thromboembolism. J Korean Med Sci. 2010; 25:1553–1559.22. Ahmad HA, Geissler A, MacLellan DG. Deep venous thrombosis prophylaxis: are guidelines being followed? ANZ J Surg. 2002; 72:331–334.23. Ibrahim EH, Iregui M, Prentice D, Sherman G, Kollef MH, Shannon W. Deep vein thrombosis during prolonged mechanical ventilation despite prophylaxis. Crit Care Med. 2002; 30:771–774.24. Bikdeli B, Sharif-Kashani B. Prophylaxis for venous thromboembolism: a great global divide between expert guidelines and clinical practice? Semin Thromb Hemost. 2012; 38:144–155.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of Complications in Critically Ill Patients
- Prevention of Venous Thromboembolism in Hip Surgery Patients
- Unexpected Multiple Organ Infarctions in a Poisoned Patient
- Clinical Year in Review of Venous Thromboembolism
- The Incidence of Venous Thromboembolism in Trauma Patients with Pelvic or Acetabular Fracture