Clin Orthop Surg.
2015 Mar;7(1):85-90. 10.4055/cios.2015.7.1.85.
Radiologic and Clinical Outcomes of Surgery in High Grade Spondylolisthesis Treated with Temporary Distraction Rod
- Affiliations
-
- 1Orthopedic Research Center, Orthopedic Department, Imam Reza Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. omidif@mums.ac.ir
- 2Addiction Research Center, Faculty of Medicine, Mashhad University of Medical Science, Mashhad, Iran.
- KMID: 2069879
- DOI: http://doi.org/10.4055/cios.2015.7.1.85
Abstract
- BACKGROUND
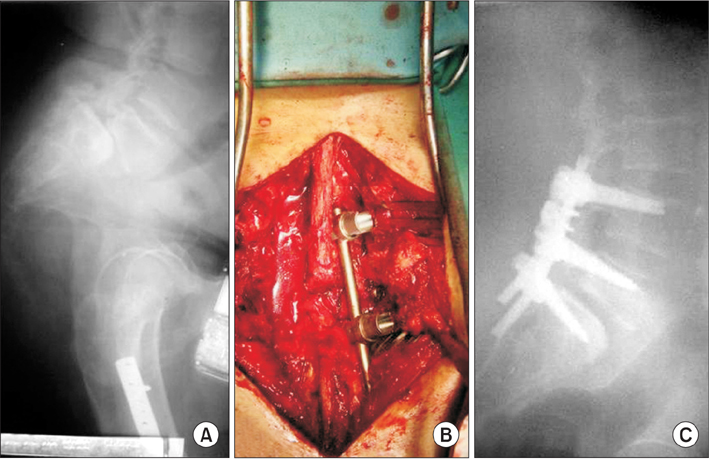
Surgical techniques used in the treatment of patients with high grade lumbar spondylolisthesis (> 50% slippage) are usually associated with a great deal of controversies. We aim to evaluate the surgical outcomes of high grade spondylolisthesis treated with an intraoperative temporary distraction rod.
METHODS
We retrospectively studied 21 patients (14 females and 7 males), aged 50.4 +/- 9.2 years, who had high grade lumbar spondylolisthesis that was treated with intraoperative temporary distraction rods, neural decompression, pedicular screw fixation, and posterolateral fusion involving one more intact upper vertebra. The mean follow-up period was 39.2 months. Radiologic and clinical outcomes were measured by slip angle, slip percentage, correction rate, Oswestry Disability Index (ODI), visual analogue scale (VAS), patient's satisfaction rate in the pre- and postoperative period. Data were analyzed by SPSS ver. 11.5.
RESULTS
Analysis of the preoperative visits and final follow-up visits indicated that surgery could improve ODI, lumbar VAS, and leg VAS from 60.5% to 8.2%, from 6.7 to 2.2, and from 6.9 to 1.3, respectively. Slip angle and slip percentage were also changed from -8degrees to -15degrees and from 59.2% to 21.4%, respectively. Mean correction rate at the final follow-up visit was 64.1%. Loss of correction was insignificant and a neurologic complication occurred in one patient due to misplacement of one screw. Excellent and good levels of satisfaction were observed in 90.5% of the patients.
CONCLUSIONS
In the surgical treatment of refractory high grade spondylolisthesis, the use of a temporary distraction rod to reduce the slipped vertebra in combination with neural decompression, posterolateral fusion, and longer instrumentation is associated with satisfactory clinical and radiologic outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Meyerding HW. Spondylolisthesis: surgical fusion of lumbosacral portion of spinal column and interarticular facets: use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg. 1956; 26(5 Part 1):566–591.2. Kasliwal MK, Smith JS, Kanter A, et al. Management of high-grade spondylolisthesis. Neurosurg Clin N Am. 2013; 24(2):275–291.
Article3. Klockner C, Weber U. Correction of lumbosacral kyphosis in high grade spondylolisthesis and spondyloptosis. Orthopade. 2001; 30(12):983–987.4. Lengert R, Charles YP, Walter A, Schuller S, Godet J, Steib JP. Posterior surgery in high-grade spondylolisthesis. Orthop Traumatol Surg Res. 2014; 100(5):481–484.
Article5. Hu SS, Bradford DS, Transfeldt EE, Cohen M. Reduction of high-grade spondylolisthesis using Edwards instrumentation. Spine (Phila Pa 1976). 1996; 21(3):367–371.
Article6. Sailhan F, Gollogly S, Roussouly P. The radiographic results and neurologic complications of instrumented reduction and fusion of high-grade spondylolisthesis without decompression of the neural elements: a retrospective review of 44 patients. Spine (Phila Pa 1976). 2006; 31(2):161–169.
Article7. Bridwell KH. Surgical treatment of high-grade spondylolisthesis. Neurosurg Clin N Am. 2006; 17(3):331–338.
Article8. Landi A, Marotta N, Mancarella C, Tarantino R, Delfini R. Trans-sacral screw fixation in the treatment of high dyplastic developmental spondylolisthesis. World J Clin Cases. 2013; 1(3):116–120.
Article9. Hart RA, Domes CM, Goodwin B, et al. High-grade spondylolisthesis treated using a modified Bohlman technique: results among multiple surgeons. J Neurosurg Spine. 2014; 20(5):523–530.
Article10. Roca J, Ubierna MT, Caceres E, Iborra M. One-stage decompression and posterolateral and interbody fusion for severe spondylolisthesis: an analysis of 14 patients. Spine (Phila Pa 1976). 1999; 24(7):709–714.
Article11. Bohlman HH, Cook SS. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach: report of two cases. J Bone Joint Surg Am. 1982; 64(3):415–418.
Article12. Kasliwal MK, Smith JS, Shaffrey CI, et al. Short-term complications associated with surgery for high-grade spondylolisthesis in adults and pediatric patients: a report from the scoliosis research society morbidity and mortality database. Neurosurgery. 2012; 71(1):109–116.
Article13. Acosta FL Jr, Ames CP, Chou D. Operative management of adult high-grade lumbosacral spondylolisthesis. Neurosurg Clin N Am. 2007; 18(2):249–254.
Article14. Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990; 13(4):227–236.
Article15. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25(22):2940–2952.
Article16. Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine (Phila Pa 1976). 2006; 31(14):E454–E459.
Article17. Goya T, Morita Y. Chronological changes in the operative indications and approaches for the treatment of spondylosis deformans of the spine. Brain Nerve. 2009; 61(6):627–635.18. Bridwell KH. Indications and techniques for anterior-only and combined anterior and posterior approaches for thoracic and lumbar spine deformities. Instr Course Lect. 2005; 54:559–565.19. Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL. Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J. 2013; 22(10):2176–2183.
Article20. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008; 90(3):656–671.21. Karampalis C, Grevitt M, Shafafy M, Webb J. High-grade spondylolisthesis: gradual reduction using Magerl's external fixator followed by circumferential fusion technique and long-term results. Eur Spine J. 2012; 21:Suppl 2. S200–S206.
Article22. Wild A, Jager M, Webb JK. Staged reposition and fusion with external fixator in spondyloptosis. Z Orthop Ihre Grenzgeb. 2001; 139(2):152–156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Result of the Posterolateral Fusion with Knodt Rod and without Knodt Rod in Spondylolysis and Spondylolisthesis of the Lumbar Spine
- Surgical Treatment of Spondylolisthesis with Knodt's Distraction Rod Instrumentation: Comparative Study with Fusion in situ
- Rectangular Rod Instrumentation in Spondylolisthesis
- Radiological Characteristics of Low-Grade Lytic Spondylolisthesis: Similarity to Dysplastic Spondylolisthesis
- Reduction of high-grade spondylolisthesis using minimally invasive spine surgery-transforaminal lumbar interbody fusion “trial-in-situ” technique: a technical note with case series