J Cerebrovasc Endovasc Neurosurg.
2015 Sep;17(3):157-165. 10.7461/jcen.2015.17.3.157.
Clinical Variables Correlated with Numbers of Intra-arterial Nimodipine Infusion in Patients with Medically Refractory Cerebral Vasospasm
- Affiliations
-
- 1Department of Neurosurgery, Daegu Catholic University, School of Medicine, Daegu, Korea. shydshyd@cu.ac.kr
- KMID: 2069238
- DOI: http://doi.org/10.7461/jcen.2015.17.3.157
Abstract
OBJECTIVE
The objective of this study was to find out the clinical variables correlated with repeated intra-arterial (IA) nimodipine infusions in patients with medically refractory cerebral vasospasm (CV) following subarachnoid hemorrhage (SAH).
MATERIALS AND METHODS
During the 36 months between January 2011 and December 2013, 275 patients were treated at our institute for SAH due to a ruptured intracranial aneurysm. Of the 275 patients, 26 patients (9.5%) met the inclusion criteria. For each patient, a retrospective review of their medical records was conducted.
RESULTS
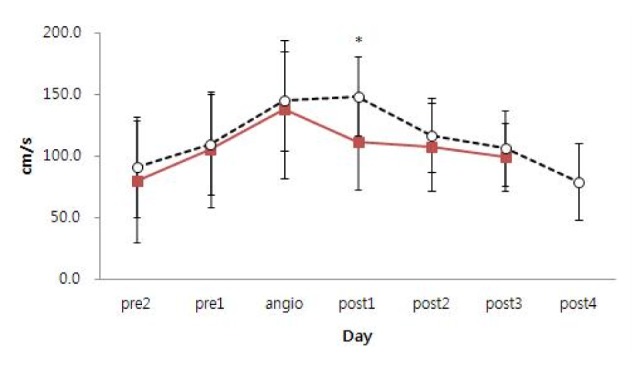
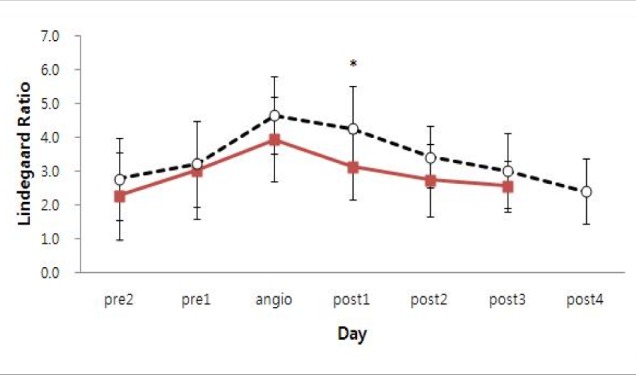
Eleven patients underwent a single IA nimodipine infusion and 15 patients underwent more than two IA nimodipine infusions. Multiple IA nimodipine infusion patients had poor improvement (2 of 15 patients, 13.3%) in Glasgow coma scale (GCS) scores after the first IA nimodipine infusion compared to patients of single IA nimodipine infusion (6 of 11 patients, 54.6%) (p = 0.038). The mean middle cerebral artery (MCA) Lindegaard ratio of multiple IA nimodipine infusion patients was 4.3 +/- 1.1 after the first IA nimodipine infusion (p = 0.039). In multiple IA nimodipine infusion patients, CV occurred more often bilaterally (p = 0.035) and distally (p = 0.001). More vessel segments were affected in multiple IA nimodipine infusion patients (3.1 +/- 1.0) (p < 0.001).
CONCLUSION
The following factors correlated with multiple IA nimodipine infusions: 1) no improvement in GCS after the IA nimodipine infusion; 2) no decrease of MCA velocity on transcranial doppler over 50 cm/s or Lindegaard ratio over 4.3 after the IA nimodipine infusion; 3) distal, bilateral, or diffuse involvement of CV.
Keyword
MeSH Terms
Figure
Reference
-
1. Baggott CD, Aagaard-Kienitz B. Cerebral vasospasm. Neurosurg Clin N Am. 2014; 7. 25(3):497–528. PMID: 24994087.
Article2. Biondi A, Ricciardi GK, Puybasset L, Abdennour L, Longo M, Chiras J, et al. Intra-arterial nimodipine for the treatment of symptomatic cerebral vasospasm after aneurysmal subarachnoid hemorrhage: preliminary results. AJNR Am J Neuroradiol. 2004; Jun-Jul. 25(6):1067–1076. PMID: 15205150.3. Cho WS, Kang HS, Kim JE, Kwon OK, Oh CW, Son YJ, et al. Intra-arterial nimodipine infusion for cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage. Interv Neuroradiol. 2011; 6. 17(2):169–178. PMID: 21696654.
Article4. Hänggi D, Turowski B, Beseoglu K, Yong M, Steiger HJ. Intra-arterial nimodipine for severe cerebral vasospasm after aneurysmal subarachnoid hemorrhage: influence on clinical course and cerebral perfusion. AJNR Am J Neuroradiol. 2008; 6. 29(6):1053–1060. PMID: 18372422.
Article5. Hop JW, Rinkel GJ, Algra A, van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. 1997; 3. 28(3):660–664. PMID: 9056628.6. Hui C, Lau KP. Efficacy of intra-arterial nimodipine in the treatment of cerebral vasospasm complicating subarachnoid haemorrhage. Clin Radiol. 2005; 9. 60(9):1030–1036. PMID: 16124986.
Article7. Kim JH, Park IS, Park KB, Kang DH, Hwang SH. Intraarterial nimodipine infusion to treat symptomatic cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J Korean Neurosurg Soc. 2009; 9. 46(3):239–244. PMID: 19844625.
Article8. Kim SS, Park DH, Lim DJ, Kang SH, Cho TH, Chung YG. Angiographic features and clinical outcomes of intra-arterial nimodipine injection in patients with subarachnoid hemorrhage-induced vasospasm. J Korean Neurosurg Soc. 2012; 9. 52(3):172–178. PMID: 23115657.
Article9. Lysakowski C, Walder B, Costanza MC, Tramer MR. Transcranial Doppler versus angiography in patients with vasospasm due to a ruptured cerebral aneurysm: A systematic review. Stroke. 2001; 10. 32(10):2292–2298. PMID: 11588316.10. Musahl C, Henkes H, Vajda Z, Coburger J, Hopf N. Continuous local intra-arterial nimodipine administration in severe symptomatic vasospasm after subarachnoid hemorrhage. Neurosurgery. 2011; 6. 68(6):1541–1547. PMID: 21311378.
Article11. Numaguchi Y, Zoarski GH, Clouston JE, Zagardo MT, Simard JM, Aldrich EF, et al. Repeat intra-arterial papaverine for recurrent cerebral vasospasm after subarachnoid haemorrhage. Neuroradiology. 1997; 10. 39(10):751–759. PMID: 9351116.
Article12. Ohkuma H, Manabe H, Tanaka M, Suzuki S. Impact of cerebral microcirculatory changes on cerebral blood flow during cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2000; 7. 31(7):1621–1627. PMID: 10884463.
Article13. Ott S, Jedlicka S, Wolf S, Peter M, Pudenz C, Merker P, et al. Continuous selective intra-arterial application of nimodipine in refractory cerebral vasospasm due to aneurysmal subarachnoid hemorrhage. Biomed Res Int. 2014; 1. 2014:970741. PMID: 24527461.
Article14. Pandey AS, Elias AE, Chaudhary N, Thompson BG, Gemmete JJ. Endovascular treatment of cerebral vasospasm: vasodilators and angioplasty. Neuroimaging Clin N Am. 2013; 11. 23(4):593–604. PMID: 24156852.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intra-arterial Nimodipine for the Treatment of Symptomatic Cerebral Vasospasm after Aneurysmal Subarachnoid Hemorrhage : Preliminary Report Clinical Research
- Effect of Intra-Arterial Nimodipine Infusion for the Treatment of Symptomatic Cerebral Vasospasm Following an Aneurysmal Subarachnoid Hemorrhage
- Endovascular Treatment of Symptomatic Vasospasm after Aneurysmal Subarachnoid Hemorrhage: A Three-year Experience
- Angiographic Features and Clinical Outcomes of Intra-Arterial Nimodipine Injection in Patients with Subarachnoid Hemorrhage-Induced Vasospasm
- The Effect of Intra-Arterial Papaverine Injection in Cerebral Vasospasm