J Korean Soc Surg Hand.
2015 Sep;20(3):96-103. 10.12790/jkssh.2015.20.3.96.
Volar Locking Plate Fixation for Distal Radius Fractures in Hemodialysis Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea. jylos@gmail.com
- 2Department of Orthopedic Surgery, Hong-Ik Hospital, Seoul, Korea.
- KMID: 2068814
- DOI: http://doi.org/10.12790/jkssh.2015.20.3.96
Abstract
- PURPOSE
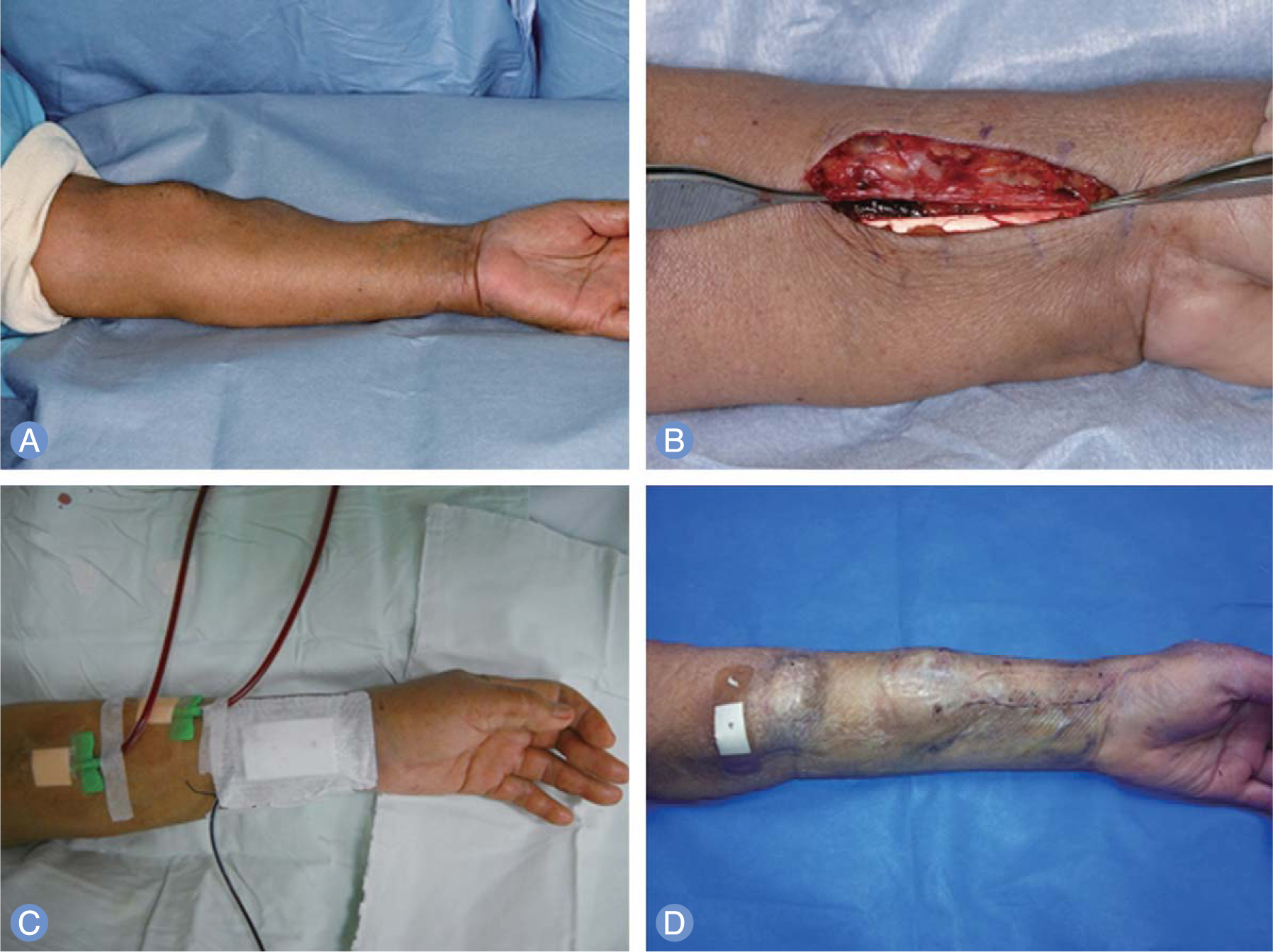
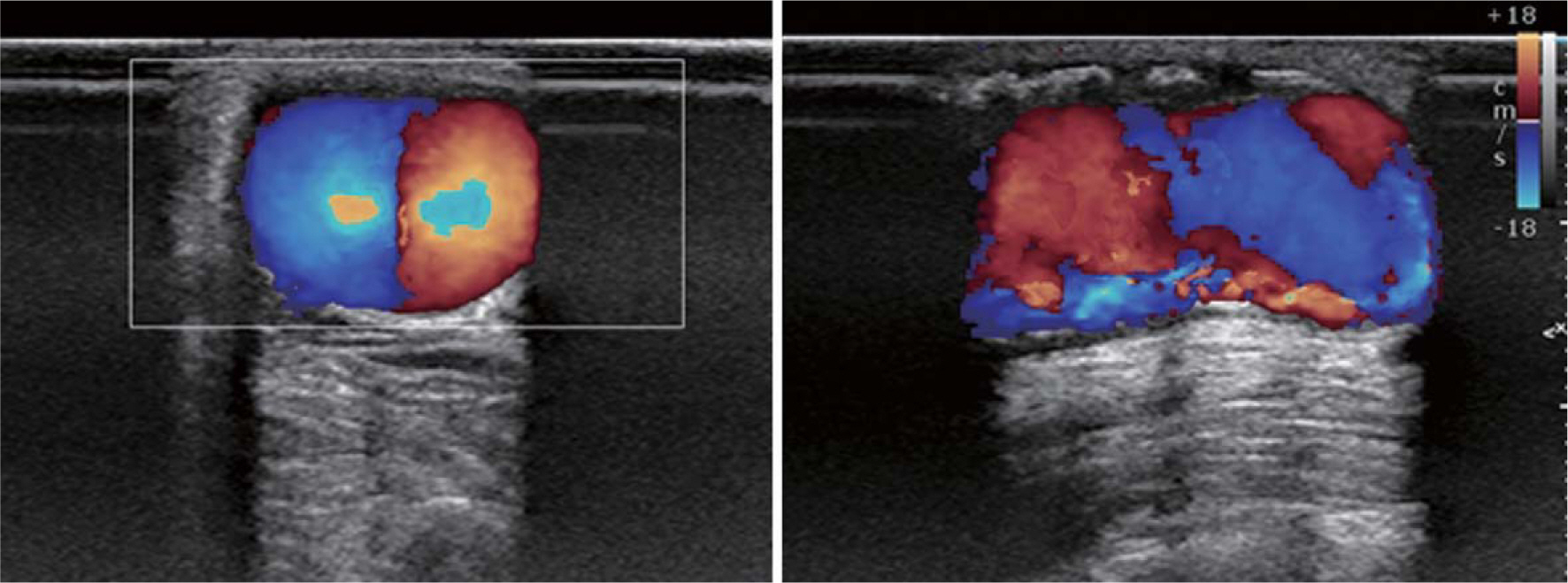
Although the possibility of distal radius fractures is strong in hemodialysis patients, there are many difficult problems such as the bleeding tendency, hypervascularity and injury to arteriovenous fistula. We studied the outcomes of open reduction and volar locking plate fixation of the distal radius fractures in hemodyalisis patients with ipsilateral arteriovenous fistula.
METHODS
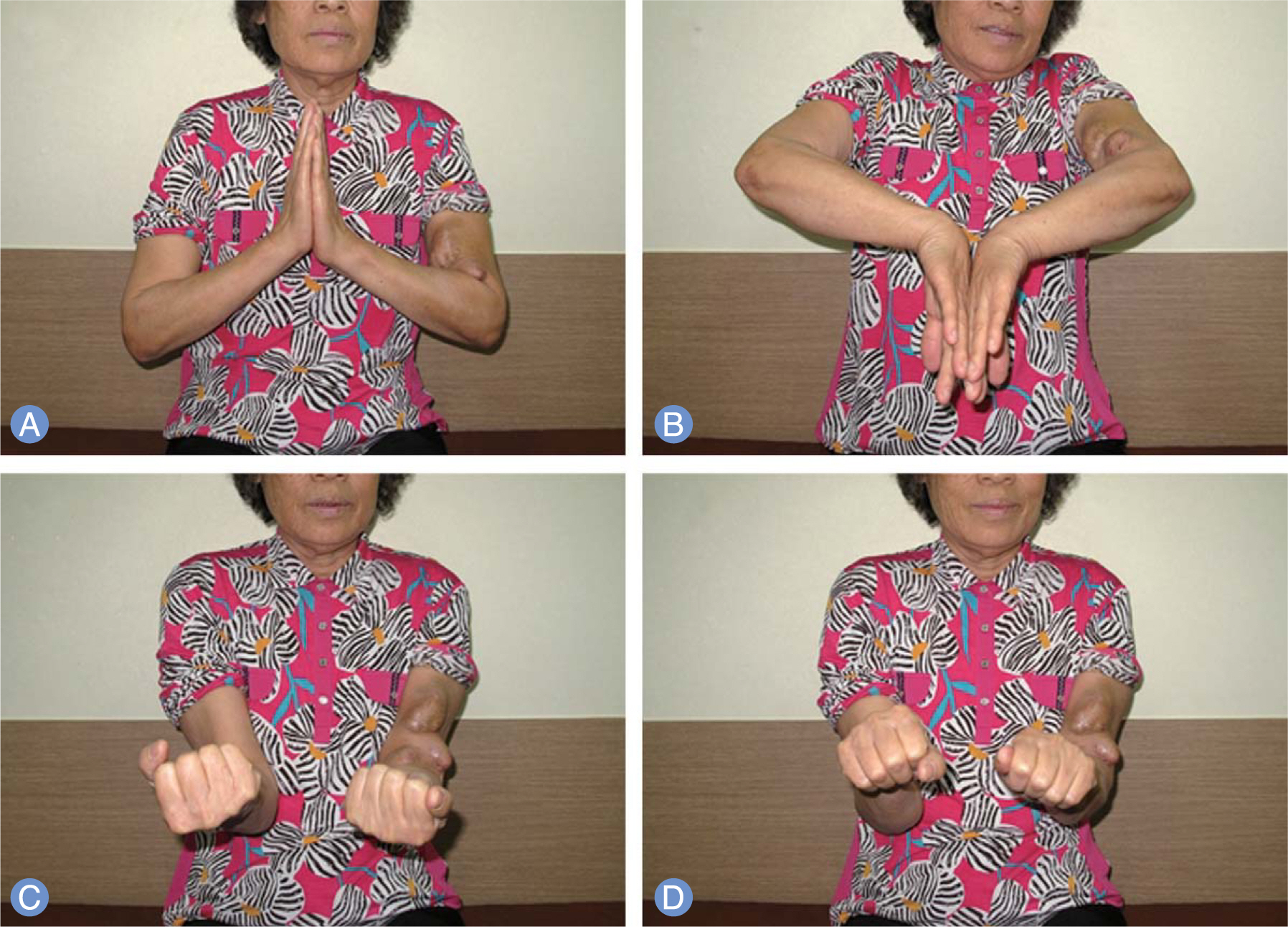
From 2007 to 2009, a retrospective chart review was performed of eleven hemodialysis patients who underwent volar locking plate fixation for treatment of distal radius fractures. Eight of them were female and three were male and mean age was 68 years (range, 57-81 years). Mean follow-up period was 19 months (range, 12-28 months). All patients had osteoporosis with mean T-score of -2.7. All operations were performed on the next day of hemodialysis. Scheduled hemodialysis was possible on the next day of surgery without splint. We analyzed radiographic results, the wrist range of motion, Mayo wrist score and disabilities of the arm, shoulder and hand (DASH) score at the last follow-up.
RESULTS
All fractures achieved anatomical reduction and united at final follow-up. Complications such as hematoma or occlusion of arteriovenous fistula were not observed. Mean Mayo wrist score was 78 and mean DASH score was 22.
CONCLUSION
Volar locking plate fixation for distal radius fractures provides immediate support for continuing hemodialysis and exercise. Open reduction of the fractures and the use of tourniquet don't seem to increase the vascular complications like hematoma and fistula occlusion.
MeSH Terms
Figure
Reference
-
References
1. Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States 2009. J Orthop Trauma. 2015; 29:e242–4.
Article2. Mehrpour SR, Nabian MH, Oryadi Zanjani L, Foroughmand-Araabi MH, Shahryar Kamrani R. Descriptive epidemiology of traumatic injuries in 18890 adults: a 5-year-study in a tertiary trauma center in iran. Asian J Sports Med. 2015; 6:e23129.
Article3. Stein EM, Kepley A, Walker M, et al. Skeletal structure in postmenopausal women with osteopenia and fractures is characterized by abnormal trabecular plates and cortical thinning. J Bone Miner Res. 2014; 29:1101–9.
Article4. Moe S, Drueke T, Cunningham J, et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2006; 69:1945–53.
Article5. Reiss E, Canterbury JM, Kanter A. Circulating parathyroid hormone concentration in chronic renal insufficiency. Arch Intern Med. 1969; 124:417–22.
Article6. Nickolas TL, Stein EM, Dworakowski E, et al. Rapid cortical bone loss in patients with chronic kidney disease. J Bone Miner Res. 2013; 28:1811–20.
Article7. Nickolas TL, McMahon DJ, Shane E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol. 2006; 17:3223–32.
Article8. Maeno Y, Inaba M, Okuno S, Yamakawa T, Ishimura E, Nishizawa Y. Serum concentrations of cross-linked N-telopeptides of type I collagen: new marker for bone resorption in hemodialysis patients. Clin Chem. 2005; 51:2312–7.
Article9. Shidara K, Inaba M, Okuno S, et al. Serum levels of TRAP5b, a new bone resorption marker unaffected by renal dysfunction, as a useful marker of cortical bone loss in hemodialysis patients. Calcif Tissue Int. 2008; 82:278–87.
Article10. Ishimura E, Okuno S, Ichii M, et al. Relationship between serum sclerostin, bone metabolism markers, and bone mineral density in maintenance hemodialysis patients. J Clin Endocrinol Metab. 2014; 99:4315–20.
Article11. Deykin D. Uremic bleeding. Kidney Int. 1983; 24:698–705.
Article12. Ishiguro S, Oota Y, Sudo A, Uchida A. Calcium phosphate cement-assisted balloon osteoplasty for a Colles' fracture on arteriovenous fistula forearm of a maintenance hemodialysis patient. J Hand Surg Am. 2007; 32:821–6.
Article13. Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures: a prospective study of thirty cases. J Bone Joint Surg Am. 1984; 66:1008–14.
Article14. Oskam J, Kingma J, Bart J, Klasen HJ. K-wire fixation for redislocated Colles' fractures. Malunion in 8/21 cases. Acta Orthop Scand. 1997; 68:259–61.15. Ludvigsen TC, Johansen S, Svenningsen S, Saetermo R. External fixation versus percutaneous pinning for unstable Colles’ fracture: equal outcome in a randomized study of 60 patients. Acta Orthop Scand. 1997; 68:255–8.
Article16. Kumbaraci M, Kucuk L, Karapinar L, Kurt C, Coskunol E. Retrospective comparison of external fixation versus volar locking plate in the treatment of unstable intra-articular distal radius fractures. Eur J Orthop Surg Traumatol. 2014; 24:173–8.
Article17. Costa ML, Achten J, Plant C, et al. UK DRAFFT: a randomised controlled trial of percutaneous fixation with Kirschner wires versus volar locking-plate fixation in the treatment of adult patients with a dorsally displaced fracture of the distal radius. Health Technol Assess. 2015; 19:1–124.
Article18. Franceschi F, Franceschetti E, Paciotti M, Cancilleri F, Maffulli N, Denaro V. Volar locking plates versus K-wire/pin fixation for the treatment of distal radial fractures: a systematic review and quantitative synthesis. Br Med Bull. 2015; 115:91–110.
Article19. Roh YH, Lee BK, Baek JR, Noh JH, Gong HS, Baek GH. A r and omized comparison of volar plate and external fixation for intra-articular distal radius fractures. J Hand Surg Am. 2015; 40:34–41.20. Williksen JH, Husby T, Hellund JC, Kvernmo HD, Rosales C, Frihagen F. External fixation and adjuvant pins versus volar locking plate fixation in unstable distal radius fractures: a randomized, controlled study with a 5-year follow-up. J Hand Surg Am. 2015; 40:1333–40.
Article21. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989; 20:208–10.
Article22. O'Banion LA, Van Buren D, Davis JW. Radiocephalic fistulas for hemodialysis: a comparison of techniques. Am Surg. 2015; 81:341–4.23. Lok CE. Fistula first initiative: advantages and pitfalls. Clin J Am Soc Nephrol. 2007; 2:1043–53.
Article24. Levin A, Bakris GL, Molitch M, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007; 71:31–8.
Article25. Kaji H, Yamauchi M, Yamaguchi T, Shigematsu T, Sugimoto T. Mild renal dysfunction is a risk factor for a decrease in bone mineral density and vertebral fractures in Japanese postmenopausal women. J Clin Endocrinol Metab. 2010; 95:4635–42.
Article26. Ball AM, Gillen DL, Sherrard D, et al. Risk of hip fracture among dialysis and renal transplant recipients. JAMA. 2002; 288:3014–8.
Article27. Boyd AS, Benjamin HJ, Asplund C. Principles of casting and splinting. Am Fam Physician. 2009; 79:16–22.28. Naito M, Ogata K, Goya T. Carpal tunnel syndrome in chronic renal dialysis patients: clinical evaluation of 62 hands and results of operative treatment. J Hand Surg Br. 1987; 12:366–74.
Article29. Salimi F. Majd Nassiri G, Moradi M, et al. Assessment of effects of upper extremity exercise with arm tourniquet on maturity of arteriovenous fistula in hemodialysis patients. J Vasc Access. 2013; 14:239–44.30. Green DP, Wolfe SW, Hotchkiss RN. et al. Green's operative hand surgery. 6th ed. Philadelphia: Elsevier Churchill Livingstone;. 2011; 15–6.31. Sugiyama Y, Naito K, Igeta Y, Obata H, Kaneko K, Obayashi O. Treatment strategy for distal radius fractures with ipsilateral arteriovenous shunts. J Hand Surg Am. 2014; 39:2265–8.
Article32. Sagedal S, Hartmann A, Sundstrom K, Bjornsen S, Fauchald P, Brosstad F. A single dose of dalteparin effectively prevents clotting during haemodialysis. Nephrol Dial Transplant. 1999; 14:1943–7.
Article33. Wilhelmsson S, Lins LE. Heparin elimination and hemostasis in hemodialysis. Clin Nephrol. 1984; 22:303–6.34. Kopec J, Gadek A, Drozdz M, et al. Carpal tunnel syndrome in hemodialysis patients as a dialysis-related amyloidosis manifestation: incidence, risk factors and results of surgical treatment. Med Sci Monit. 2011; 17:CR505–9.35. Williksen JH, Husby T, Hellund JC, Kvernmo HD, Rosales C, Frihagen F. External fixation and adjuvant pins versus volar locking plate fixation in unstable distal radius fractures: a randomized, controlled study with a 5-year follow-up. J Hand Surg Am. 2015; 40:1333–40.
Article36. Strohm PC, Muller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures: a randomized trial. J Bone Joint Surg Am. 2004; 86:2621–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Failure of Distal Locking Screws in an Intraarticular Distal Radius Fracture Treated with Volar Locking Plate Fixation
- External Fixation for Distal Radius Fractures
- Relationship between the Length of Distal Locking Screws and Diaphyseal Screws in Volar Plate Fixation of Distal Radius Fractures
- Volar Plating of Distal Radius Fractures
- Radiologic Results in Accordance with the Number of Distal Locking Screws in Volar Plate Fixation for Distal Radius Fractures