J Gynecol Oncol.
2009 Mar;20(1):17-21. 10.3802/jgo.2009.20.1.17.
Differing prognosis of cervical cancer patients with high risk of treatment failure after radical hysterectomy warrants trial treatment modification
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ajou University Hospital, Suwon, Korea. hsryu@ajou.ac.kr
- 2Department of Radiation Oncology, Ajou University Hospital, Suwon, Korea.
- KMID: 2055643
- DOI: http://doi.org/10.3802/jgo.2009.20.1.17
Abstract
OBJECTIVE
The aim of this study was to ascertain whether all cervical cancer patients who received adjuvant concurrent chemoradiation (CCRT) for high risk of treatment failure after radical hysterectomy are at the same risk of treatment failure, and if not, to propose trial treatment modification.
METHODS
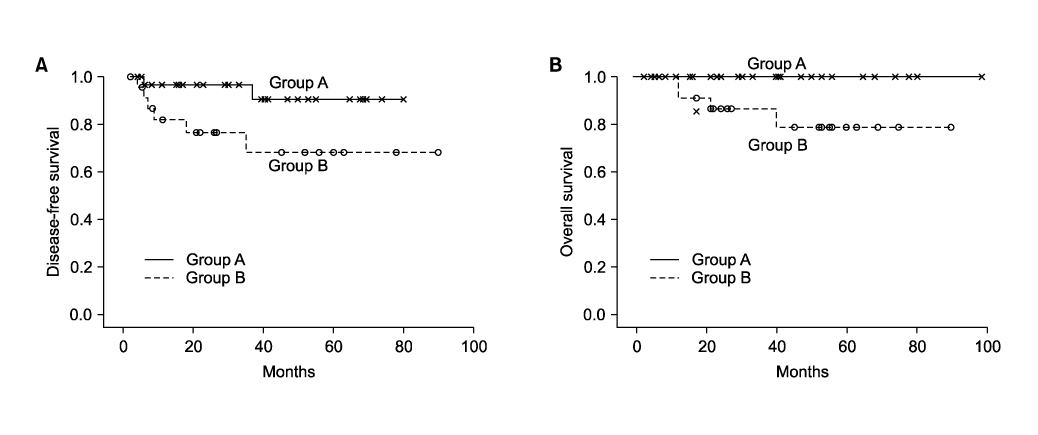
Between January 1999 and December 2007, 58 patients with FIGO stage Ib-IIa cervical cancer received adjuvant CCRT due to high risk factors such as positive lymph nodes or positive parametrium, or positive vaginal resection margins. Patients were divided into two Groups. Group A were patients with negative parametrium, negative vaginal resection margins, and only unilateral lymph node metastasis (involved L/N< or =2). Group B were those with either bilateral pelvic lymph node involvement, or more than 2 lymph node involvement, or positive parametrium with lymph node involvement.
RESULTS
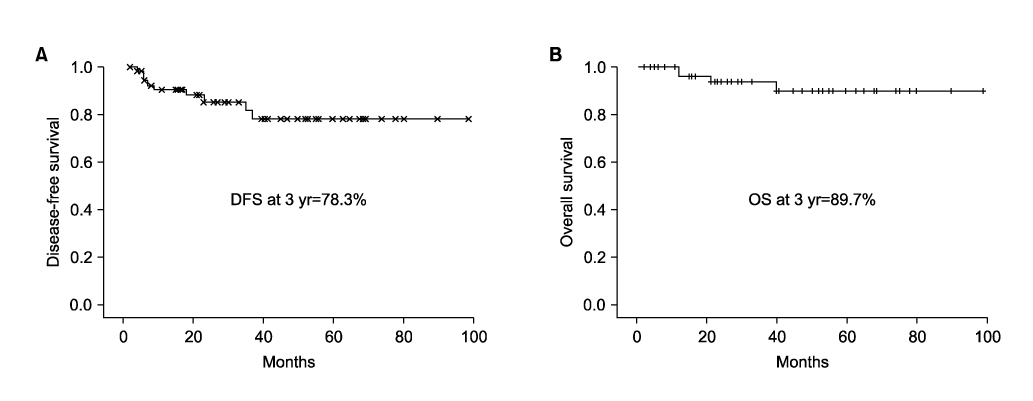
During a median follow-up period of 34 months (range, 6 to 102 months), 9 patients (15.5%) experienced recurrence; among whom 2 patients (2/28, 7.1%) were Group A, and 7 patients (7/30, 23.3%) were Group B. At 3 years, the estimated progression-free survival rate of all 58 patients was 78.3%, and the overall survival rate was 89.7%. Patients in Group A had significantly better progression-free survival (88.2% vs. 68.2%, p=0.042) and overall survival rate (100% vs. 78.8%, p=0.034) than Group B.
CONCLUSION
Treatment modifications such as consolidation chemotherapy after CCRT may be considered based on the poor prognosis of very high risk patients such as those patients in Group B.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prognostic Value of Log Odds of Positive Lymph Nodes after Radical Surgery Followed by Adjuvant Treatment in High-Risk Cervical Cancer
Jeanny Kwon, Keun-Yong Eom, In Ah Kim, Jae-Sung Kim, Young-Beom Kim, Jae Hong No, Kidong Kim
Cancer Res Treat. 2016;48(2):632-640. doi: 10.4143/crt.2015.085.
Reference
-
1. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000. 18:1606–1613.2. Piver MS, Chung WS. Prognostic significance of cervical lesion size and pelvic node metastases in cervical carcinoma. Obstet Gynecol. 1975. 46:507–510.3. Hsu CT, Cheng YS, Su SC. Prognosis of uterine cervical cancer with extensve lymph node metastases: special emphasis on the value of pelvic lymphadenectomy in the surgical treatment of uterine cervical cancer. Am J Obstet Gynecol. 1972. 114:954–962.4. Nahhas WA, Sharkey FE, Whitney CW, Husseinzadeh N, Chung CK, Mortel R. The prognostic significance of vascular channel involvement and deep stromal penetration in early cervical carcinoma. Am J Clin Oncol. 1983. 6:259–264.5. Martimbeau PW, Kjorstad KE, Iversen T. Stage IB carcinoma of the cervix, the Norwegian Radium hospital: II. Results when pelvic nodes are involved. Obstet Gynecol. 1982. 60:215–218.6. Van Nagel JR Jr, Donaldson ES, Parker JC, Van Dyke AH, Wood EG. The prognostic significance of cell type and lesion size in patients with cervical cancer treated by radical surgery. Gynecol Oncol. 1977. 5:142–151.7. Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990. 38:352–357.8. Inoue T, Morita K. The prognostic significance of number of positive nodes in cervical carcinoma stages IB, IIA, and IIB. Cancer. 1990. 65:1923–1927.9. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.10. Ryu HS, Chun M, Chang KH, Chang HJ, Lee JP. Postoperative adjuvant concurrent chemoradiotherapy improves survival rates for high-risk, early stage cervical cancer patients. Gynecol Oncol. 2005. 96:490–495.11. Morice P, Castaigne D, Pautier P, Rey A, Haie-Meder C, Leblanc M, et al. Interest of pelvic and paraaortic lymphadenectomy in patients with stage IB and II cervical carcinoma. Gynecol Oncol. 1999. 73:106–110.12. Michel G, Morice P, Castaigne D, Leblanc M, Rey A, Duvillard P. Lymphatic spread in stage Ib and II cervical carcinoma: anatomy and surgical implications. Obstet Gynecol. 1998. 91:360–363.13. Samlal RA, van der Velden J, Schilthuis MS, Gonzalez Gonzalez D, Ten Kate FJ, Hart AA, et al. Identification of high-risk Groups among node-positive patients with stage IB and IIA cervical carcinoma. Gynecol Oncol. 1997. 64:463–467.14. Tinga DJ, Timmer PR, Bouma J, Aalders JG. Prognostic significance of single versus multiple lymph node metastases in cervical carcinoma stage IB. Gynecol Oncol. 1990. 39:175–180.15. Stock RG, Chen AS, Flickinger JC, Kalnicki S, Seski J. Node-positive cervical cancer: impact of pelvic irradiation and patterns of failure. Int J Radiat Oncol Biol Phys. 1995. 31:31–36.16. Lin HH, Cheng WF, Chan KW, Chang DY, Chen CK, Huang SC. Risk factors for recurrence in patients with stage IB, IIA, and IIB cervical carcinoma after radical hysterectomy and postoperative pelvic irradiation. Obstet Gynecol. 1996. 88:274–279.17. Wertheim MS, Hakes TB, Daghestani AN, Nori D, Smith DH, Lewis JL Jr. A pilot study of adjuvant therapy in patients with cervical cancer at high risk of recurrence after radical hysterectomy and pelvic lymphadenectomy. J Clin Oncol. 1985. 3:912–916.18. Houvenaeghel G, Lelievre L, Rigouard AL, Buttarelli M, Jacquemier J, Viens P, et al. Residual pelvic lymph node involvement after concomitant chemoradiation for locally advanced cervical cancer. Gynecol Oncol. 2006. 102:74–79.19. Choi CH, Lee JW, Kim TJ, Kim WY, Nam HR, Kim BG, et al. Phase II study of consolidation chemotherapy after concurrent chemoradiation in cervical cancer: preliminary results. Int J Radiat Oncol Biol Phys. 2007. 68:817–822.20. Wong LC, Choo YC, Choy D, Sham JS, Ma HK. Long-term follow-up of potentiation of radiotherapy by cis-platinum in advanced cervical cancer. Gynecol Oncol. 1989. 35:159–163.21. Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology Group trial (RTOG) 90-01. J Clin Oncol. 2004. 22:872–880.22. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999. 17:1339–1348.23. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differing prognosis of cervical cancer patients with high risk of treatment failure after radical hysterectomy: To the editor
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- The influence of number of high risk factors on clinical outcomes in patients with early-stage cervical cancer after radical hysterectomy and adjuvant chemoradiation
- Recent Management of FIGO stage IB2 Cervical Cancer
- Vaginal evisceration after radical hysterectomy and adjuvant radiation