Hip Pelvis.
2013 Jun;25(2):95-101. 10.5371/hp.2013.25.2.95.
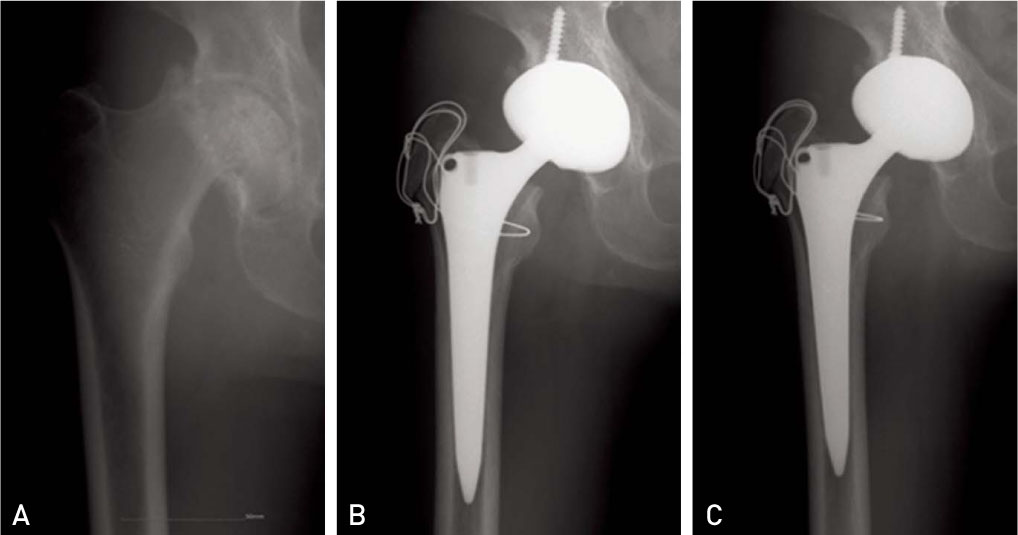
Ceramic on Ceramic Cementless Total Hip Arthroplasty with a 36 mm Diameter Femoral Head: More than Three Years Follow up
- Affiliations
-
- 1Department of Orthopedic Surgery, Ilsan Paik Hospital, College of Medicine, Inje University, Goyang, Korea. osd11@paik.ac.kr
- KMID: 2054145
- DOI: http://doi.org/10.5371/hp.2013.25.2.95
Abstract
- PURPOSE
The purpose of this study was to analyze the results for clinical outcome and radiologic assessment of ceramic on ceramic cementless total hip arthroplasty using a 36 mm diameter femoral head.
MATERIALS AND METHODS
This study included a group of 40 patients of 43 cases who underwent ceramic on ceramic cementless total hip arthroplasty using a 36 mm diameter femoral head. The age range of this group was 28 to 82(mean 56); we monitored them over a period of 5.3 years(3-7.5 years). This clinical evaluation process included monitoring the degree of pain, range of motion, and the Harris hip score after three years since the surgery was performed. Radiographic evaluation and complication were confirmed as well.
RESULTS
The preoperative Harris hip score increased from 43.4(21-57) to 88.1(81-95) after the surgery. The average motion range of hip was 113degrees flexion, 30degrees abduction, 24degrees adduction, 36degrees external rotation, and 12degrees internal rotation. Subjective pain was zero or minimal in all cases. Among the complications, dislocation occurred in only one case by a fall from a height and was reduced by closed reduction. There was no occurrence of ceramic fracture, even though infection occurred in one hip.
CONCLUSION
The clinical outcome and radiologic assessment of the ceramic on ceramic cementless total hip arthroplasty using a 36 mm diameter femoral head showed a satisfactory result at three-year follow-up. Longer-term follow up is needed for further assessment.
Keyword
MeSH Terms
Figure
Reference
-
1. Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970; 72:7–21.
Article2. Harris WH. The problem is osteolysis. Clin Orthop Relat Res. 1995; (311):46–53.3. Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation. Four to seven-year results. J Bone Joint Surg Am. 2000; 82:789–798.
Article4. Han CD, Choi CJ, Yang IH, Lee DH. Total hip arthroplasty with ceramic-on-ceramic Articulation: minimum 5-year follow-up results. J Korean Orthop Assoc. 2006; 41:421–427.
Article5. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.
Article6. Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004; 19:387–390.
Article7. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article8. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.9. Joshi RP, Eftekhar NS, McMahon DJ, Nercessian OA. Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J Bone Joint Surg Br. 1998; 80:585–590.10. Maloney WJ, Jasty M, Harris WH, Galante JO, Callaghan JJ. Endosteal erosion in association with stable uncemented femoral components. J Bone Joint Surg Am. 1990; 72:1025–1034.
Article11. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632.12. Herrlin K, Selvik G, Pettersson H, Lidgren L. Range of motion caused by design of the total hip prosthesis. Acta Radiol. 1988; 29:701–704.
Article13. Synder M, Drobniewski M, Sibiński M. Long-term results of cementless hip arthroplasty with ceramic-on-ceramic articulation. Int Orthop. 2012; 36:2225–2229.
Article14. Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplasty. 2001; 16:1071–1074.
Article15. Restrepo C, Parvizi J, Kurtz SM, Sharkey PF, Hozack WJ, Rothman RH. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008; 23:643–649.
Article16. Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999; 14:509–513.
Article17. Herrlin K, Pettersson H, Selvik G, Lidgren L. Femoral anteversion and restricted range of motion in total hip prostheses. Acta Radiol. 1988; 29:551–553.
Article18. Herrlin K, Selvik G, Pettersson H, Kesek P, Onnerfält R, Ohlin A. Position, orientation and component interaction in dislocation of the total hip prosthesis. Acta Radiol. 1988; 29:441–444.
Article19. Dorr LD, Wolf AW, Chandler R, Conaty JP. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res. 1983; (173):151–158.
Article20. Amstutz HC, Lodwig RM, Schurman DJ, Hodgson AG. Range of motion studies for total hip replacements. A comparative study with a new experimental apparatus. Clin Orthop Relat Res. 1975; (111):124–130.21. Grzegorzewski A, Kozlowski P, Synder M, Domzalski M. The use of Bicontact hip prosthesis in treatment of coxarthrosis. Chir Narzadow Ruchu Ortop Pol. 2001; 66:435–441.22. Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty. A five-year minimum follow-up study. J Bone Joint Surg Am. 2005; 87:530–535.23. Kim DJ, Ki SC, Park KH, Kim YH, Chung YY. Total hip arthroplasty using a ceramic on ceramic bearing surfaces. J Korean Orthop Assoc. 2008; 43:495–500.
Article24. Ha YC, Kim SY, Kim HJ, Yoo JJ, Koo KH. Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasy. Clin Orthop Relat Res. 2007; 458:106–110.
Article25. Hasegawa M, Sudo A, Hirata H, Uchida A. Ceramic acetabular liner fracture in total hip arthroplasty with a ceramic sandwich cup. J Arthroplasty. 2003; 18:658–661.
Article26. Walter WL, O'toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007; 22:496–503.27. Lombardi AV Jr, Skeels MD, Berend KR, Adams JB, Franchi OJ. Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clin Orthop Relat Res. 2011; 469:1547–1553.
Article28. Jameson SS, Lees D, James P, et al. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Joint Surg Br. 2011; 93:876–880.29. Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ). 1995; 24:347–351.30. Seo GT. Leg length discrepancy in total hip arthroplasty. J Korean Hip Soc. 2002; 14:308–311.31. Park WR, Moon KP, Suh KT. Leg length discrepancy after total hip arthroplasty. J Korean Hip Soc. 2010; 22:20–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ceramic on Ceramic Cementless Total Hip Arthroplasty Using a Large Diameter Head
- Ceramic-on-Ceramic Bearing Total Hip Arthroplasty: Five-Year Midterm Follow-up Results
- A Case of Failure of a Ceramic Head in Total Hip Arthroplasty: A Case Report
- Ceramic on Sandwich Ceramic Bearing Primary Cementless Total Hip Arthroplasty (Result of 2 to 5 years follow up)
- Short-term Results of Cementless Ceramic-on-ceramic Articulation Total Hip Arthroplasty