Hip Pelvis.
2012 Sep;24(3):250-255. 10.5371/hp.2012.24.3.250.
Traumatic Recurrent Dislocation of the Hip with Bankart Type Lesion: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Chungbuk National University, Cheongju, Korea. hcshon@hanmail.net
- KMID: 2054140
- DOI: http://doi.org/10.5371/hp.2012.24.3.250
Abstract
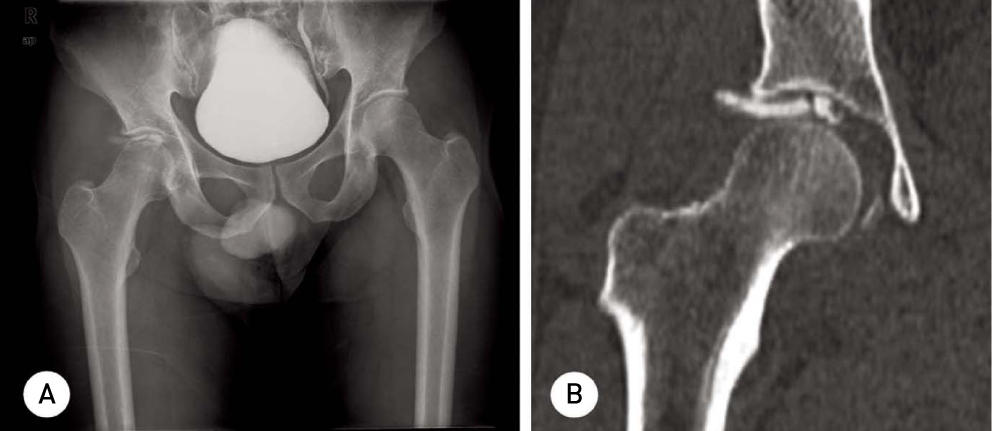
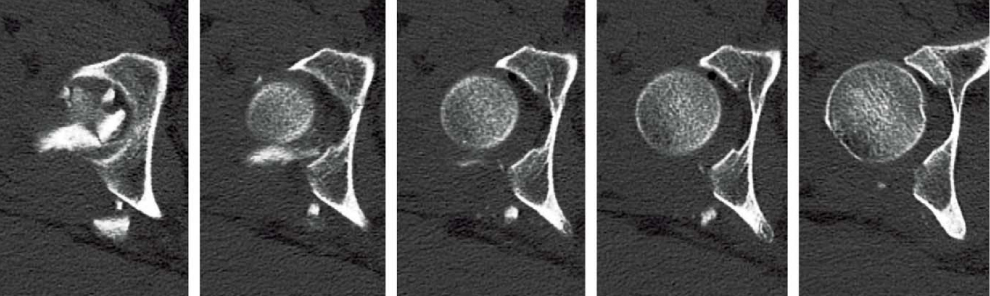
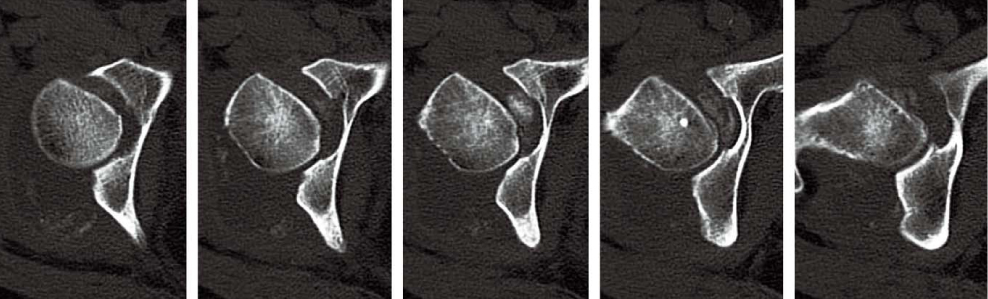
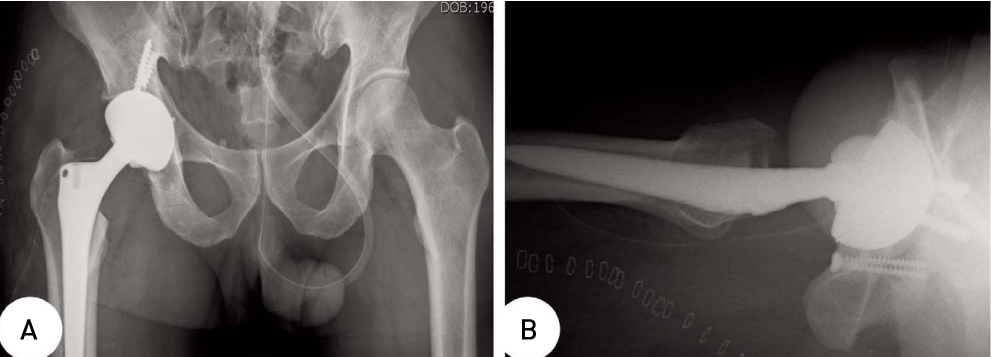
- The recurrent dislocation of hip in adult can be uncommonly induced by neuromuscular disease or dysplasia of hip. But in the case of traumatic dislocation of hip with acetabular fracture, the possibility of recurrent dislocation can be decreased if treated with accurate fixation or traction. We have experienced a case of hip dislocation with comminuted acetabular fracture, which was treated only with soft tissue suture and without fixation because of severity of the acetabular fracture. An inappropriate conservative management was done during the post operation period, eventually result in recurrent dislocation and degeneration of posterior wall and head of femur which resembled bony Bankart lesion of the shoulder. The reduction was not able to be maintained, as a result THRA was done. A year after the operation, good prognosis was found in replaced hip without any recurrent dislocation.
MeSH Terms
Figure
Reference
-
1. Heeg M, Klasen HJ, Visser JD. Operative treatment for acetabular fractures. J Bone Joint Surg Br. 1990. 72:383–386.
Article2. Schlickewei W, Elsasser B, Mullaji AB, Kuner EH. Hip dislocation without fracture: traction or mobilization after reduction? Injury. 1993. 24:27–31.
Article3. Keith JE Jr, Brashear HR Jr, Guilford WB. Stability of posterior fracture-dislocations of the hip. Quantitative assessment using computed tomography. J Bone Joint Surg Am. 1988. 70:711–714.
Article4. Olson SA. The computerized tomography subchondral arc: a new method of assessing acetabular articular continuity after fracture (a preliminary report). J Orthop Trauma. 1993. 7:402–413.
Article5. Marchetti ME, Steinberg GG, Coumas JM. Intermediate-term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma. 1996. 10:455–461.
Article6. Daum WJ. Traumatic posterior acetabular defects reconstructed with iliac crest autograft. A report of two cases. Clin Orthop Relat Res. 1993. (291):188–192.7. Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003. (407):173–186.
Article8. Weber M, Ganz R. Recurrent traumatic dislocation of the hip: report of a case and review of the literature. J Orthop Trauma. 1997. 11:382–385.
Article9. Marti RK, Kloen P. Chronic recurrent posterior dislocation of the hip after a Pipkin fracture treated with intertrochanteric osteotomy and acetabuloplasty. A case report. J Bone Joint Surg Am. 2000. 82:867–872.
Article10. Lieberman JR, Altchek DW, Salvati EA. Recurrent dislocation of a hip with a labral lesion: treatment with a modified Bankart-type repair. Case report. J Bone Joint Surg Am. 1993. 75:1524–1527.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Traumatic Anterior Dislocation of the Hips: A Case Report
- Clinical Outcome after Surgical Treatment of Recurrent Shoulder Dislocation with Small Bony Bankart
- C. T. arthrography on Bankart lesion
- Author's proposed classification of the bankart lesion to traumatic recurrent anterior shoulder dislocation(Rhee's arthroscopic classification of the bankart lesion in TUBS)
- Traumatic Hip Dislocation in a Three-year-old Child: A Case Report