Tuberc Respir Dis.
2013 May;74(5):215-221. 10.4046/trd.2013.74.5.215.
Identification and Distribution of Nontuberculous Mycobacteria from 2005 to 2011 in Cheonan, Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea.
- 2Department of Laboratory Medicine, Dankook University College of Medicine, Cheonan, Korea. insoo@dankook.ac.kr
- KMID: 2050889
- DOI: http://doi.org/10.4046/trd.2013.74.5.215
Abstract
- BACKGROUND
Nontuberculous mycobacteria (NTM) are considered opportunistic pathogens, and several species of NTM are associated with human diseases that typically involve the pulmonary, skin/soft tissue, or lymphatic systems; such infection may also cause disseminated diseases. Recent studies have reported increasing rates of NTM-induced disease worldwide.
METHODS
Respiratory samples are being analyzed for acid-fast bacilli (AFB) culture and NTM identification at Dankook University Hospital in Cheonan, Korea, from September 2005 to September 2011. Identification is performed by using polymerase chain reaction-restriction fragment length polymorphism analysis targeting a novel region of the rpoB gene.
RESULTS
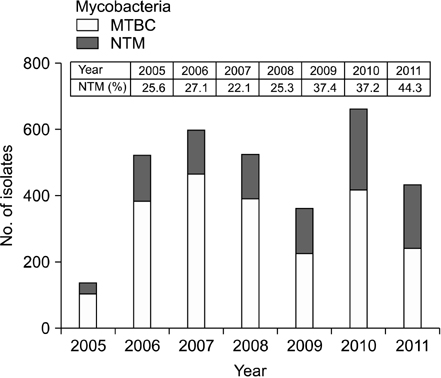
A total of 25,133 specimens were received for AFB culture, of which 1,014 (4.0%) were NTM-positive. A total of 267 samples from 186 patients were tested for NTM identifications, and 232 samples from 157 patients were positive for NTM species. Among the patients who tested positive for NTM, 65.6% were men and the average age was 63.3 years. Mycobacterium avium complex, the most commonly detected NTM pathogen, was found in 65.9% of the 232 samples. The annual average percentage of NTM isolates from AFB culture-positive specimens was 31.3%: the highest rate was seen in 2011 (44.3%), followed by 2009 (37.4%) and 2010 (37.2%). An upward trend in NTM incidence was found during the study period.
CONCLUSION
The prevalence of pulmonary NTM isolates continues to increase in Cheonan, suggesting that pulmonary NTM disease is becoming increasingly common.
MeSH Terms
Figure
Cited by 1 articles
-
Infection Source and Epidemiology of Nontuberculous Mycobacterial Lung Disease
Doosoo Jeon
Tuberc Respir Dis. 2019;82(2):94-101. doi: 10.4046/trd.2018.0026.
Reference
-
1. Katoch VM. Infections due to non-tuberculous mycobacteria (NTM). Indian J Med Res. 2004; 120:290–304.2. Portaels F. Epidemiology of mycobacterial diseases. Clin Dermatol. 1995; 13:207–222.3. Primm TP, Lucero CA, Falkinham JO 3rd. Health impacts of environmental mycobacteria. Clin Microbiol Rev. 2004; 17:98–106.4. Olivier KN. Nontuberculous mycobacterial pulmonary disease. Curr Opin Pulm Med. 1998; 4:148–153.5. Jeong J, Lee SH, Jeong US, Chang CL, Kim SR. Identification of mycobacteria using high performance liquid chromatography in clinical specimens. Korean J Clin Microbiol. 2004; 7:148–155.6. Bang HI, Choi TY, Shin JW. Comparison of Ogawa media, BACTEC MGIT 960 system and TB/NTM real-time PCR for detecting Mycobacterium species. Tuberc Respir Dis. 2011; 71:249–253.7. Koh WJ, Kwon OJ, Ham HS, Suh GY, Chung MP, Kim HJ, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens. Korean J Med. 2003; 65:10–21.8. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000; 38:2966–2971.9. Lee H, Bang HE, Bai GH, Cho SN. Novel polymorphic region of the rpoB gene containing Mycobacterium species-specific sequences and its use in identification of mycobacteria. J Clin Microbiol. 2003; 41:2213–2218.10. Shin S, Kim EC, Yoon JH. Identification of nontuberculous mycobacteria by sequence analysis of the 16S ribosomal RNA, the heat-shock protein 65 and the RNA polymerase beta-subunit genes. Korean J Lab Med. 2006; 26:153–160.11. Daley CL, Griffith DE. Nontuberculous mycobacterial infections. In : Mason RJ, Broaddus VC, Martin TR, King TE, Schraufnagel DE, Murray JE, editors. Murray and Nadel's textbook of respiratory medicine. 5th ed. Philadelphia: Saunders;2010. p. 793–810.12. Brown-Elliott BA, Griffith DE, Wallace RJ Jr. Newly described or emerging human species of nontuberculous mycobacteria. Infect Dis Clin North Am. 2002; 16:187–220.13. Marras TK, Chedore P, Ying AM, Jamieson F. Isolation prevalence of pulmonary non-tuberculous mycobacteria in Ontario, 1997-2003. Thorax. 2007; 62:661–666.14. Lai CC, Tan CK, Chou CH, Hsu HL, Liao CH, Huang YT, et al. Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000-2008. Emerg Infect Dis. 2010; 16:294–296.15. Thomson RM. NTM working group at Queensland TB Control Centre and Queensland Mycobacterial Reference Laboratory. Changing epidemiology of pulmonary nontuberculous mycobacteria infections. Emerg Infect Dis. 2010; 16:1576–1583.16. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, et al. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005; 9:1046–1051.17. Lee JY, Choi HJ, Lee H, Joung EY, Huh JW, Oh YM, et al. Recovery rate and characteristics of nontuberculous mycobacterial isolates in a university hospital in Korea. Tuberc Respir Dis. 2005; 58:385–391.18. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, et al. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010; 14:1069–1071.19. Lee J, Kim Y, Park J, Ko W, Yang D, Kim S, et al. Clinical utility of bronchial washing PCR for IS6110 and amplicor for the rapid diagnosis of active pulmonary tuberculosis in smear negative patients. Tuberc Respir Dis. 2001; 50:213–221.20. Choi SP, Lee BK, Min JH, Kim JH. Pathogenic classification and clinical characteristics of nontuberculous mycobacterial pulmonary disease in a national tuberculosis hospital. Tuberc Respir Dis. 2005; 59:606–612.21. Baek SH, Lee JM, Kang MJ, Son JW, Lee SJ, Kim DG, et al. How reliable is sputum PCR test in the diagnosis of pulmonary tuberculosis when sputum smear is negative? Tuberc Respir Dis. 2001; 50:222–228.22. Lee JS, Ji HS, Hong SB, Oh YM, Lim CM, Lee SD, et al. Clinical utility of polymerase chain reaction for the differentiation of nontuberculous mycobacteria in patients with acid-fast bacilli smear-positive specimens. Tuberc Respir Dis. 2005; 58:452–458.23. Kim HK, Kim YR, Park JP, Kim NH, Ok CH, Jung MH, et al. Isolation of nontuberculous mycobacteria by DNA probe and clinical characteristics of patients with NTM pulmonary disease. Tuberc Respir Dis. 2005; 58:248–256.24. Simons S, van Ingen J, Hsueh PR, Van Hung N, Dekhuijzen PN, Boeree MJ, et al. Nontuberculous mycobacteria in respiratory tract infections, eastern Asia. Emerg Infect Dis. 2011; 17:343–349.25. Andrejak C, Thomsen VO, Johansen IS, Riis A, Benfield TL, Duhaut P, et al. Nontuberculous pulmonary mycobacteriosis in Denmark: incidence and prognostic factors. Am J Respir Crit Care Med. 2010; 181:514–521.26. Prevots DR, Shaw PA, Strickland D, Jackson LA, Raebel MA, Blosky MA, et al. Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am J Respir Crit Care Med. 2010; 182:970–976.27. Douglas JG, Calder MA, Choo-Kang YF, Leitch AG. Mycobacterium gordonae: a new pathogen? Thorax. 1986; 41:152–153.28. Asija A, Prasad A, Eskridge E. Disseminated Mycobacterium gordonae infection in an immunocompetent host. Am J Ther. 2011; 18:e75–e77.29. Yim JJ, Park YK, Lew WJ, Bai GH, Han SK, Shim YS. Mycobacterium kansasii pulmonary diseases in Korea. J Korean Med Sci. 2005; 20:957–960.30. Kim KS, Shin YD, Ahn JW. Epidemiologic study of unclassified mycobacteria. Tuberc Respir Dis. 1966; 13:5–20.31. Lee SK, Shin YD. Epidemiologic study of atypical mycobacterial infection. Tuberc Respir Dis. 1967; 14:12–38.32. Lee HW, Kim MN, Shim TS, Bai GH, Pai CH. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients. Tuberc Respir Dis. 2002; 53:173–182.33. Lee JK, Kwon HY, Kwon JK, Lee HJ, Lee DW, Lee YJ, et al. Recovery rate of nontuberculous mycobacteria and the clinical course of nontuberculous mycobacterial pulmonary disease at a secondary hospital. Tuberc Respir Dis. 2009; 67:199–204.34. Lee MK, Seo YH, Jeong JH, Park PW, Kim KH, Ahn JY, et al. Nontuberculous mycobacteria isolated from respiratory specimens during recent two years: distribution and clinical significance. Korean J Clin Microbiol. 2012; 15:98–103.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Identification of Mycobacteria using High Performance Liquid Chromatography in Clinical Specimens
- Clinical Evaluation of 10 Cases of Nontuberculous Mycobacteria Isolated from Sputum
- Culture and Identification of Mycobacteria by Biphasic Media and Multiplex PCR/PCR-RFLP
- Increasing Burden of Nontuberculous Mycobacteria in Korea
- Delayed Nontuberculous Mycobacterium Manifestation 1 Year after a Dog Bite on the Hand